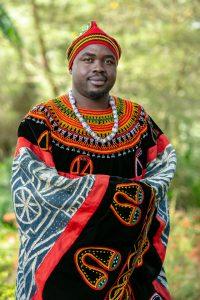
 Dr. Justin Komguep Nono is a Cameroonian immunoparasitologist recognised for his research on host–helminth interactions, specifically how helminths modulate immune and vaccine responses. He heads the Laboratory of Molecular Biology and Biotechnology and the Immunobiology of Helminth Infections Unit at the Institute of Medical Research and Medicinal Plant Studies (IMPM) of the Ministry of Scientific Research and Innovation in Yaoundé, Cameroon. A former Honorary Senior Lecturer at the University of Cape Town, he holds leadership roles in the Global Schistosomiasis Alliance (GSA), the Cameroon Immunology Society (CIS), and the Federation of African Immunological Societies (FAIS). His contributions to infectious disease research in Africa have earned him accolades and research funds from the European and Developing Countries Clinical Trials Partnership (EDCTP), the African Academy of Sciences (AAS), the UK Royal Society, the Welcome Centre from Integrative Parasitology and the Centre for International Development of the University of Glasgow (UK) and the Global Health R&D of Merck Healthcare, Ares Trading S.A., (a subsidiary of Merck KGaA, Darmstadt, Germany).
Dr. Justin Komguep Nono is a Cameroonian immunoparasitologist recognised for his research on host–helminth interactions, specifically how helminths modulate immune and vaccine responses. He heads the Laboratory of Molecular Biology and Biotechnology and the Immunobiology of Helminth Infections Unit at the Institute of Medical Research and Medicinal Plant Studies (IMPM) of the Ministry of Scientific Research and Innovation in Yaoundé, Cameroon. A former Honorary Senior Lecturer at the University of Cape Town, he holds leadership roles in the Global Schistosomiasis Alliance (GSA), the Cameroon Immunology Society (CIS), and the Federation of African Immunological Societies (FAIS). His contributions to infectious disease research in Africa have earned him accolades and research funds from the European and Developing Countries Clinical Trials Partnership (EDCTP), the African Academy of Sciences (AAS), the UK Royal Society, the Welcome Centre from Integrative Parasitology and the Centre for International Development of the University of Glasgow (UK) and the Global Health R&D of Merck Healthcare, Ares Trading S.A., (a subsidiary of Merck KGaA, Darmstadt, Germany).
What initially drew you to this field?
My journey into helminth research began by chance, but it quickly grew into a deep passion. Working with Professor Klaus Brehm at the University of Würzburg, I was introduced to Echinococcus multilocularis, a model helminth with remarkable biological features. What caught me was the idea of a parasite harbouring immortal cells, something both disturbing and fascinating. That experience led me to explore the broader story of host–helminth co-evolution, and how these organisms have developed tools to thrive within their hosts. Along the way, I’ve been inspired by researchers such as Prof. Manfred Lutz, Prof. Frank Brombacher, and Prof. Rick Maizels, among others, whose work continually reaffirms the importance of this field.
What are the critical gaps in helminth research, and how can the global health community better prioritise neglected tropical diseases (NTDs)?
Helminths are among the best storytellers of human evolution. Through them, we can learn so much about how the immune system functions, and malfunctions. Yet, research into helminths remains underfunded and overlooked. We still don’t fully understand how chronic helminth infections affect vaccine responses, or how they might be harnessed to treat inflammatory diseases. These are huge, missed opportunities. If we genuinely want to improve global health, especially in resource-limited settings, we must prioritise these parasites not only for the harm they cause, but for the insights they can offer into human biology and immunity.
How has your research contributed to changing perceptions about the role of parasites in immune modulation? Are there emerging therapeutic strategies that excite you?
Our research brought forward a critical finding: chronic Schistosoma mansoni infections deplete immune memory cells in the bone marrow. These are the very cells that maintain long-term vaccine protection. What shocked us was that previously vaccinated individuals were losing immunity to diseases like measles and polio, simply because of persistent helminth infection. However, what excited me was that deworming, which cleared the parasites and allowed immune memory to recover. That’s powerful. It suggests that by integrating deworming into immunisation programs, we can restore and even enhance vaccine effectiveness. This is a simple, low-cost approach with huge public health potential.
You’ve been recognised with several fellowships. How have these shaped your career or opened new collaborations?
Fellowships have been defining moments in my journey. From the German Research Foundation to the Sydney Brenner Fellowship, EDCTP, the African Academy of Sciences, the UK Royal Society, Merck KGaA and others, each one opened new doors. They gave me visibility, access to global networks, and opportunities to lead or co-lead major research initiatives. More importantly, they came with responsibility, an expectation to use my platform not just for science, but for mentorship, collaboration, and impact. I’ve come to see scientific recognition as a means to an end: to support work that matters, and to train the next generation to do even better.
How do you balance academic rigour with the urgency of real-world health challenges in Africa?
For me, it’s always “impact over recognition.” Although, these are not mutually exclusive, I have had frequent encouragement (strong ones, thus the mention here) from my oldest collaborators i.e. Dr Thomas Spangenberg and Dr Claudia Demarta-Gatsi on striving first for research that addresses real problems in our communities. If planned well from the beginning, it is now my experience that rigour and timely relevance can go hand in hand. In Africa, we face infrastructural and funding limitations, but we also have deep wells of creativity. We learn to solve complex problems with limited resources. That’s where collaboration, both local and global, becomes crucial. It fills the gaps and pushes the work forward, even when the conditions aren’t ideal.
What leadership lessons have you learned, and how do you mentor young African scientists?
One of the most significant lessons is that leadership is more than science; it’s about vision, structure, and human connection. I always advise young researchers to start with mentors who can provide them with close guidance early on and later seek out established scientists who can open doors to the international stage. But mentorship alone isn’t enough. We must also work with institutions, administrators, finance, and policymakers to build systems that support research in the long term. No one will build that for us. Once you establish that structure and demonstrate your value, support begins to emerge from governments, funders, and partners.
How can African immunologists contribute to solving global health challenges?
The answer is simple: collaboration. We need to move beyond the “rockstar scientist” model. Real and sustainable progress comes from strong institutions, committed teams, and shared goals. African immunologists have a great deal to offer, but we need to work together, across countries, disciplines, and generations. That also means prioritising mentorship and building networks through our national and regional societies. If we train the next generation to collaborate and lead, our collective impact will reach far beyond the continent. As a rule of thumb, I usually advocate for every established scholar on the continent to strive to train a minimum of 50 graduate students into research before retirement: I believe this to be the most sustainable approach to ensure Africa global competitiveness and relevance in solving present and future local as well as global health challenges.
Looking ahead, what are your hopes for the future of immunology in Africa?
Immunology is advancing rapidly, and the tools and infrastructure required are becoming increasingly expensive and complex. Africa must invest more seriously in research, or risk being left behind. The COVID-19 pandemic exposed a painful truth; we lacked the capacity to develop our own vaccines and so we were forced to follow the agenda (not always in our interest) of those who could. That must change! The next decade should focus on vaccine development from Africa, where infectious diseases are more prevalent, especially in understanding and robustly setting (local) correlates of protection to ensure maximal efficacy in our settings. This will require partnerships between scientists, clinicians, and manufacturers. Vaccines remain the most cost-effective tools in public health, and if Africa invests now, the regular threats from infectious agents on the continent should certainly encourage our growth to become leaders in developing and delivering these needed tools – for the well-being of Africa, the sovereignty of Africa’s health agenda and consequently a better global health system for humankind.
Interview by Faith Oluwamakinde










