- Patient presentation
- History
- Differential Diagnosis
- Examination
- Investigations
- Discussion
- Evaluation - Questions & answers
- MCQ
- References
Patient presentation
A 9 year old girl of mixed racial ethnicity with a recurrent history of mycobacterial disease presents to a tertiary hospital with a persistently painful, swollen left ankle responding slowly to indicated treatment. She has no other pain but generally feels tired and has a poor appetite.
Acknowledgement
This case study was kindly provided by Dr Justyna Wojno, from Groote Schuur Hospital, Western Cape
Three months ago she presented for the first time with an active arthritis in her left ankle, which prevented her from walking. S.aureus was cultured from a tissue biopsy, antibiotic susceptibility testing was done and the patient was put on a course of indicated antibiotics for 6 weeks (two weeks parentral and four weeks oral). Although she appeared to have been compliant on treatment her improvement was minimal.
She continued oral treatment for a further three months after which the joint finally started to settle. The swelling is almost completely resolved and she is able to walk for short distances.
She is also currently on treatment for Mycobacterium avium intracellulare (MAI)
• Rifampicin 450mg daily
• Ethambutol 600mg daily
• Ofloxacin 400mg daily
• Ethionamide 375mg daily
• Clarithromycin 250mg bd
• Pyridoxine 25mg daily
• Folate 5mg daily
• Multivitamin 1 tab daily
Past Medical History
Age 6 months: Patient diagnosed with M.tuberculosis infection although her mother was unsure if it was pulmonary or disseminated TB. She completed treatment.
Age 8 years: Patient diagnosed with M.tuberculosis infection which was confirmed as Pulmonary TB by patient’s mother. She completed treatment.
Age 8 years 10 months: Patient presented again with symptoms of Pulmonary TB. She was admitted to hospital and started on treatment for multi-drug resistant –TB (MDR-TB) as she was initially thought to have MDR-TB with this being her third episode of infection. However, culture of a pus swab from a lymph node abscess and a sputum sample revealed the pus swab to be acid fast bacilli (AFB) negative and culture positive for M.tuberculosis and non- M.tuberculosis resembling Mycobacterium avium intracellulare (MAI). The sputum specimen was AFB negative and culture positive for Non- M. tuberculosis (not speciated further). Her therapy was changed to MAI treatment (see above).
Age 9 years: Patient presented with arthritis of the left ankle. A biopsy was taken which cultured S. aureus and the patient received antibiotics for 6 weeks, but the joint hardly responded to treatment. Tissue biopsy from the joint was sent for TB culture and histology. Both results were non-contributory. The histology showed active inflammation with no granuloma formation and the culture was negative for mycobacteria.
Family History
No family members with TB or chronic disease.
Vaccinations
Not available
Social
Patient has both parents and 3 siblings. However, she has not been visited by her family as there are social problems and has thus been staying at St Josephs, a home for children with chronic illnesses. She has also been admitted to numerous hospitals and other children’s homes prior to staying at St Josephs.
Allergies
None known
Medications
No additional medication or traditional medicine
Differential Diagnosis
Primary or acquired immunodeficiencies increase the susceptibility to mycobacterial infection, therefore the following should be considered:
- HIV
- Diabetes
- Childhood leukaemia
- Cystic Fibrosis
- Severe combined immunodecficiency (SCID)
- X-linked hyper IgM syndrome
- Chronic Granulomatous disease
- Ectodermal dysplasia with immunodeficiency
- Mendelian susceptibility to mycobacterial disease, especially in tuberculosis-naïve populations where a lack of selection exhibits a greater susceptibility to disease.
The genetic aetiologies include:
- IFN-γR1 deficiency
- IFN-γR2 deficiency
- STAT-1 deficiency
- IL-12Rβ1 deficiency
- IL-12p40 deficiency
- CD40 signaling and NEMO
Examination
Patient is a thin, unhappy and unhealthy looking child, walking with an antalgic gait, favouring her right side.
Vital signs
Apyrexial, normal blood pressure and heart rate, normal respiratory rate
General
- Pale conjunctiva and noticeable proptosis of left eye, but patient has not reported any eye symptoms or changes.
- No lymphadenopathy, but scarring from previous cervical lymph node abscess visible
- Weight- 21.5kg (3rd centile)
- Height-25th centile
CVS
Nil of Note
Respiratory System
- No abnormalities detected
- No signs of respiratory distress
- Normal breath sounds
Abdomen
- Soft and non-tender
- No organomegaly
- Normal bowel sounds
Musculoskeletal system
- Antalgic gait favouring the right side
- Left ankle mildly swollen, warm and tender. Full range of motion intact but painful at extremes of movement.
- No joint crepitations
CNS
- Higher function intact
- No motor or sensory deficits
- No cerebellar signs
- Antalgic gait
Ophthalmology
The slight proptosis of the left orbit has been assessed by an opthalmologist who postulated that this could be a congenital finding. However, in light of the most recent bone scan results, a local bone lesion of infectious aetiology cannot be excluded.
Investigations
| FBC: | ||
|---|---|---|
| WBC | 21.25 | (3.9 – 10.2 x 10ˆ9/l) |
| Hb | 11.7 | (11.8 – 14.6 g/dl) |
| MCV | 65.3 | (77 -91.5 fl) |
| MCH | 21.6 | (25.8 – 31.7 pg) |
| MCHC | 33 | (33 – 35 g/dl) |
| ESR | 115 | |
| Hypochromic , microcytic anaemia | ||
| Differential: | ||
| Neutrophils | 67.5 | (33 – 55%) |
| Lymphocytes | 25.7 | (33 – 50%) |
| Monocytes, easinophils and basophils | Normal | |
| Absolute: | ||
| Neutrophils | 14.34 | (1.45 – 5.2 x 10ˆ9/l) |
| Lymphocytes | 5.46 | (1.5 – 4.2 x 10ˆ9/l) |
HIV
Negative
Neutrophil oxidative burst test
Normal
Lymphocyte Stimulation test
PHA, ConA and Pokeweed responses normal. Protein A response (B cells) is less than 50% of 2 adult controls and Candida (pure protein antigen response) is abnormally low.
Immunoglobulin levels
IgG 19.8 (6-20g/l)
IgA 1.77 (0,8-3g/l)
IgM 2.1 (0,4-1,8g/l)
Sweat test
23 (0-60mmol/l)
Bence-jones proteins in urine
Absent
A bone-scan and bone marrow tests were conducted to assess for a disseminated/ chronic cause for the patient’s current features.
Bone scan
A three phase bone scan and spec-CT of the thoracic and lumbar spine showed widespread areas of abnormal uptake/ ‘hot spots’. Areas affected include: skull including the orbits, shoulders, ribs, multiple vertebrae, pelvis, femur and tibia as well as the left ankle.This could possibly indicate disseminated infection such as atypical mycobacterial infection. Patient has not complained of pain in the muskuloskeletal system other than of the left ankle.
Bone marrow
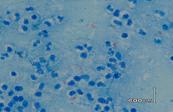
Histology showed hypercellular reactive changes with no evidence of malignancy or granuloma formation.
Discussion
In the past it was thought that most recurrent TB was due to reactivation as opposed to re-infection. It is now well described that in fact, relapse is the most common mechanism of recurrence, especially in areas such as the Western Cape (South Africa) where the prevalence of TB is extremely high, up to 40% of recurrent TB is due to reinfection and the rest is due to relapse (Vega et al., 2021.)
How then does one assess whether recurrent tuberculosis, in a child, is merely re-infection, or related to an immunodeficiency that may predispose one to invasive, disseminated and/or recurrent infections? One way to know would be to use genetic sequencing, however this requires sequencing during primary infection and during recurrence, which is a seldom technique used in primary health care. Infections due to bacilli Calmette-Guerin (BCG) or non-tuberculous mycobacteria (NTM), also known as Mycobacteria other than tuberculosis (MOTT), that are recurrent or disseminated are highly suggestive of impaired immunity. In this case our patient most likely did not receive her BCG vaccination as no infection with M.bovis was isolated.
While BCG immunisation of infants affords moderate protection against extra-pulmonary TB, it can also reveal unsuspected disorders of immune function. Effective containment of live, attenuated BCG bacilli requires intact T-lymphocyte and macrophage function. In the absence of effective host immune function, injected bacilli can proliferate unchecked and spread throughout the body. Unresolved infection at the injection site and its spread to regional lymph nodes can be early indicators of host immunodeficiency, although regional adenopathy alone is relatively common among immunocompetent children. With disseminated infection, the tissues most severely affected are usually the liver, spleen, bone marrow, and lungs. Despite the susceptibility of BCG organisms to most anti-TB medications, the response to treatment is generally poor without immune reconstitution. Massive numbers of organisms are usually evident and concurrent infections with CMV, fungi, and bacteria often occur, adding to the challenges of patient management.
- HIV
- Diabetes
- Childhood leukaemia
- Bone marrow or organ transplantation
- Cystic Fibrosis
Primary immunodeficiency (PID) should be considered in a child with recurrent mycobacterial disease. Not all PID’s are associated with a predisposition to mycobacterial infections. One must understand the basis of the immunity necessary to combat mycobacterial organisms to help one understand why this susceptibility occurs. Very briefly, mycobacterial immunity requires a functioning T-cell response with functioning macrophage/IL12/IFN-gamma interactions. Thus, there are numerous genes coding for the products responsible for this complex immune interaction. Polymorphisms/mutations in these genes may thus result in immune dysfunction. The following PID’s have an increased susceptibility to mycobacterial disease:
- Severe combined immunodecficiency: is an autosomal recessive disorder that is fatal within in the first two year of aninfant’s life unless immune restoring treatment is received, such as transplants of blood-forming stem cells, gene therapy or enzyme therapy (Severe Combined Immunodeficiency (SCID) | NIH: National Institute of Allergy and Infectious Diseases, 2019). Various phenotypic variations of the disease occur but all types are associated with a lack of T-cells with or without B-cell level alterations. These patients can present with local or disseminated post-BCG vaccine infection. Infection with NTM is also described.
- X-linked hyper IgM syndrome: a genetic disorder of T cells. Mutation (in the gene encoding CD154) results in impaired T-cell/ antigen presenting cell interaction. These patients can get disseminated M.tuberculosis or NTM infections.
- Chronic Granulomatous disease: mutations (in the genes encoding NADPH oxidase subunits) affect the phagocytes’ ability to destroy ingested microorganisms. These patients are predisposed to (among other things) M.tuberculosis and NTM infections.
- Ectodermal dysplasia with immunodeficiency: mutation in the NEMO gene involved in developmental and immunological pathways that are thus affected downstream. Patients are predisposed to M.tuberculosis and NTM.
- Mendelian susceptibility to mycobacterial disease (MSMD): unlike the other PID’s these patients develop mainly severe, disseminated mycobacterial disease. One must remember that the majority of the population have effective innate resistance to mycobacteria and even though almost a third of the world’s population is infected with M.tuberculosis, only 10% will ever develop disease. Is this then a genetic predisposition? Many may argue that social and environmental factors play the most important part, but literature shows that host genetics do play a role. It has been shown that tuberculosis-naïve populations, due to lack of selection, exhibit greater susceptibility to disease. MSMD mainly affects the IL-12/IFN-g.
The genetic aetiology: (Thus far described)
- IFN-γR1 deficiency
- IFN-γR2 deficiency
- STAT-1 deficiency
- IL-12Rβ1 deficiency
- IL-12p40 deficiency
- CD40 signalling and NEMO
It is clear then that there is quite a complex interaction between the host, environment and organism. Therefore, immunodeficiency must be considered in a patient with unusual susceptibility to mycobacteria.
Download images for this case
Evaluation – Questions & answers
What is the diagnosis?
In the absence of genetic testing what evidence contributes to a diagnosis of Mendelian susceptibility to mycobacterial disease?
Recurrent mycobacterial infections, absent lymphadenopathy and the lack of granulomatous formation as evidenced by “normal” histological findings. Due to the disruption of the INF-g circuit caused by MSMD, the QuantiFeron blood test can be used to assess the release of INF-g in an individual that is known to have been actively infected by Mycobacterium tuberculosis.
What is the normal immune response to Mycobacteria?
Immune control of mycobacterial infections requires a cell mediated immune response because mycobacteria are intracellular pathogens. The immune response is initiated by activation of CD4+ T helper cells following phagocytosis of free mycobacteria by dendritic cells and macrophages (alveolar). Dendritic cells then produce IL-12 which in turn promotes the differentiation of CD4+ helper T cells to IL-2 and IFN-γ producing Th1 phenotypes. IL-2 is required for activation of CD8+ cytotoxic T Lymphocytes that mediate killing of mycobacteria infected macrophages.
What role does IFN-γ have in the normal immune response to mycobacteria?
INF-γ enhances phagocytosis of free mycobacteria and antigen presentation of mycobacterial proteins to T cells. IFN-g also plays a crucial role in granuloma formation to mitigate the dissemination of the bacterium throughout the body and is important for phagosome-lysosome fusion (Ghanavi et al., 2021). Which cells do mycobacteria infect? Mycobacteria are intracellular pathogens of macrophages, in particular macrophages of lung tissue.
Download images for this case
Multiple Choice Questions
Earn 1 HPCSA or 0.25 SACNASP CPD Points – Online Quiz
Download images for this case
References
- Ghanavi, J., Farnia, P., Farnia, P., & Velayati, A. (2021). The role of interferon-gamma and interferon-gamma receptor in tuberculosis and nontuberculous mycobacterial infections. International Journal of Mycobacteriology, 10(4), 349–357. https://doi.org/10.4103/IJMY.IJMY_186_21
- Severe Combined Immunodeficiency (SCID) | NIH: National Institute of Allergy and Infectious Diseases. (2019). Retrieved October 26, 2023, from https://www.niaid.nih.gov/diseases-conditions/severe-combined-immunodeficiency-scid
- Vega, V., Rodríguez, S., Van Der Stuyft, P., Seas, C., & Otero, L. (2021). Recurrent tuberculosis: a systematic review and meta-analysis of the incidence rates and the proportions of relapse and reinfection. https://doi.org/10.1136/thoraxjnl-2020-215449