- Patient presentation
- History
- Differential Diagnosis
- Examination
- Investigations
- Discussion
- Treatment
- Final Outcome
- References
- Evaluation - Questions & answers
- MCQ
A 19 month old infant presents with marked leg swelling, pain and inability to walk within 6 hours of receiving booster vaccinations
Acknowledgement
This case study was kindly provided by Dr Guy de Bruyn MBBCh, MPH from the Perinatal HIV Research Unit, Chris Hani Baragwanath Hospital, Soweto.
History
- Infant was a healthy 19 month old female who developed marked right thigh swelling, redness and pain within 6 hours of receiving booster vaccinations.
- At the visit to the clinic she received a booster dose of diphtheria, pertussis and tetanus in her right thigh, a booster dose of conjugated Haemophilus vaccine in the left thigh and trivalent oral polio vaccine administered by mouth.
- She had received her primary immunisation series at 6, 10 and 14 weeks of age, consisting of trivalent oral polio vaccine administered by mouth, hepatitis B virus vaccine, Haemophilus vaccine and diphtheria, pertussis and tetanus vaccine.
- No prior adverse reactions had been noted.
- No childhood or other illnesses noted.
Differential Diagnosis
- administration error
- pyomyositis
- hypersensitivity reaction
- generalised swelling reactions
- localised abscess
- extensive limb swelling (ELS)
- idiopathic
Examination
Vitals:
Temperature: 38.5 ˚C
Respiratory rate, blood pressure and heart rate: nil of note
Clinical Findings:
Marked swelling of the right thigh, with redness and tenderness
No discernable swelling noted in the left thigh
No generalised oedema
Investigations
- Ultrasound examinations demonstrated swelling of both the subcutaneous and muscle layers of the vaccinated leg.
- Repeat ultrasound examination after 48 hours showed considerable resolution of muscle swelling, compared with subcutaneous tissue swelling.
- Although ultrasound is not typically done, it performed to rule out localised abscess formation.
Discussion
Hypersensitivity Reactions
 There are 4 main types of hypersensitivity reactions, and one subtype, namely:
There are 4 main types of hypersensitivity reactions, and one subtype, namely:
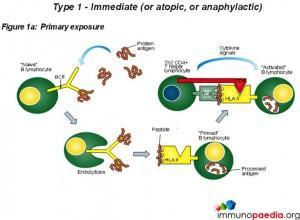
- Type 1 – immediate (or atopic, or anaphylactic)
- Type 2 – antibody-dependent
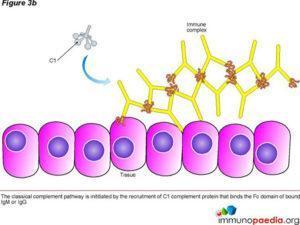
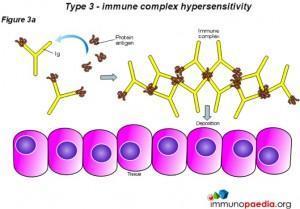
- Type 3 – immune complex
- Type 4 – cell-mediated (Delayed-Type Hypersensitivity, DTH)
- A possible type 5 hypersensitivity reaction has been suggested, however more research is yet to be done to determine whether it is a completely separate category of its own or a variation of a type 2 response (Millar, 2021)– stimulatory (can be used to distinguish from classical type 2)
In this discussion we will briefly look at each type of reaction and then discuss type 3 hypersensitivity in more detail with emphasis on a response known as the Arthus reaction.
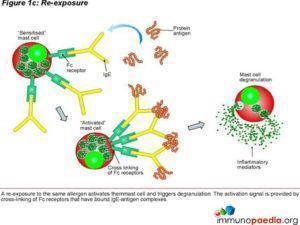
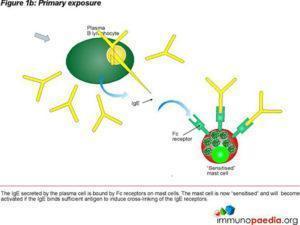 Type 1 hypersensitivity is an allergic reaction provoked by reexposure to a specific type of antigen referred to as an allergen. Exposure may be by ingestion, inhalation, injection, or direct contact. The difference between a normal immune response and a type I hypersensitivity response is that plasma cells secrete IgE. This class of antibody binds to the Fc receptors on the surface of tissue mast cells and blood basophils. Mast cells and basophils coated by IgE are then “sensitised.” Subsequent exposure to the same allergen cross-link the bound IgE on sensitised cells resulting in degranulation and secretion of pharmacologically active mediators such as histamine, leukotriene, and prostaglandin. The principal effects of these products are vasodilation and smooth-muscle contraction which may act locally or systemically. Symptoms vary from mild irritation to anaphylactic shock. Treatment usually involves epinephrine, antihistamines, and hyposensitization (Persaud, Memon and Savliwala, 2022).
Type 1 hypersensitivity is an allergic reaction provoked by reexposure to a specific type of antigen referred to as an allergen. Exposure may be by ingestion, inhalation, injection, or direct contact. The difference between a normal immune response and a type I hypersensitivity response is that plasma cells secrete IgE. This class of antibody binds to the Fc receptors on the surface of tissue mast cells and blood basophils. Mast cells and basophils coated by IgE are then “sensitised.” Subsequent exposure to the same allergen cross-link the bound IgE on sensitised cells resulting in degranulation and secretion of pharmacologically active mediators such as histamine, leukotriene, and prostaglandin. The principal effects of these products are vasodilation and smooth-muscle contraction which may act locally or systemically. Symptoms vary from mild irritation to anaphylactic shock. Treatment usually involves epinephrine, antihistamines, and hyposensitization (Persaud, Memon and Savliwala, 2022).
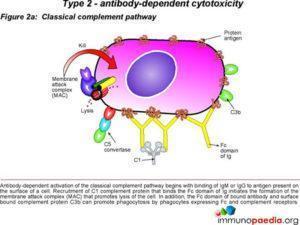
 In type 2 hypersensitivity, the antibodies produced by the immune response bind to antigens on the patient’s own cell surfaces. These antigens may either be intrinsic (“self” antigen) or extrin
In type 2 hypersensitivity, the antibodies produced by the immune response bind to antigens on the patient’s own cell surfaces. These antigens may either be intrinsic (“self” antigen) or extrin
sic where the antibodies are absorbed onto the cells during exposure to some foreign antigen, possibly as part of infection with a pathogen. These cells are recognised by macrophages or dendritic cells which act as antigen presenting cells. This then results in a B cell response where antibodies are produced against the foreign antigen. A well known example is the reaction to penicillin where the drug binds to red blood cells causing them to be seen as different and antibodies to the drug are produced by B cell proliferation. IgG and IgM antibodies bind to these antigens to form complexes that activate the classical pathway of complement activation for eliminating cells presenting foreign antigens. In this process mediators of acute inflammation are generated at the site and membrane attack complexes cause cell lysis and death. This occurs within hours.
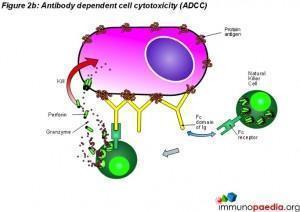
 Another form of type 2 hypersensitivity is called Antibody Dependent Cell Mediated Cytotoxicity (ADCC). Here, cells exhibiting foreign antigen are tagged with either IgG or IgM antibodies which are then recognised by Natural Killer (NK) cells and macrophages and destroyed. Conditions that result from type 2 HS reactions include; Immune Thrombocytopenia (ITP), Autoimmune Hemolytic anemia (AIHA), Autoimmune Neutropenia, Hemolytic Disease of the Fetus and the Newborn, Goodpasture Syndrome and pemphigus (Justiz Vaillant, Vashisht and Zito, 2022).
Another form of type 2 hypersensitivity is called Antibody Dependent Cell Mediated Cytotoxicity (ADCC). Here, cells exhibiting foreign antigen are tagged with either IgG or IgM antibodies which are then recognised by Natural Killer (NK) cells and macrophages and destroyed. Conditions that result from type 2 HS reactions include; Immune Thrombocytopenia (ITP), Autoimmune Hemolytic anemia (AIHA), Autoimmune Neutropenia, Hemolytic Disease of the Fetus and the Newborn, Goodpasture Syndrome and pemphigus (Justiz Vaillant, Vashisht and Zito, 2022).
 In type 3 hypersensitivity, soluble immune complexes (aggregations of antigens and IgG and IgM antibodies) form in the blood and are deposited in various tissues such as the skin, the kid
In type 3 hypersensitivity, soluble immune complexes (aggregations of antigens and IgG and IgM antibodies) form in the blood and are deposited in various tissues such as the skin, the kid
neys and the joints. They then trigger an immune response according to the classical pathway of complement activation. There are two stages relating to the development of the complexes. Firstly the complex forms when IgG and IgM antibodies are bound to an antigen, thereafter the complexes form larger complexes. It is at the first stage of this formation where clearance by monocytes or macrophages is not possible and the antigen-antibody complexes release vasoactive amines that increase the permeability of vasculature promoting their spread and deposit as stated above (Yalew,2020). The reaction takes hours to days to develop. The immune complexes trigger an inflammatory cascade similar to what is seen in serum sickness and Arthus reaction (Justiz Vaillant, Vashisht and Zito, 2022).
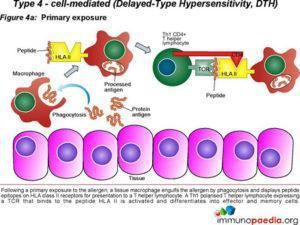
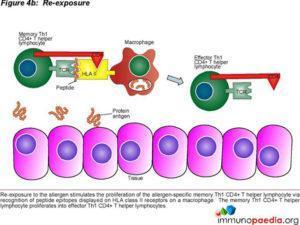
 Type 4 hypersensitivity is often called the delayed type as the reaction takes two to three days to develop. Unlike the first three types already discussed, this reaction is not antibody mediated but rather a type of cell-mediated response. CD8+ cytotoxic T cells and CD4+ helper T cells recognise antigen in a complex with either type 1 or 2 major histocompatibility complex. The antigen-presenting cells in this case are macrophages which secrete IL-1, which stimulates the proliferation of further CD4+ T cells. CD4+ T cells secrete IL-2 and interferon gamma, further inducing the release of other Type 1 cytokines, thus mediating the immune response. Activated CD8+ T cells destroy target cells on contact while activated macrophages produce hydrolytic enzymes and, on presentation with certain intracellular pathogens, transform
Type 4 hypersensitivity is often called the delayed type as the reaction takes two to three days to develop. Unlike the first three types already discussed, this reaction is not antibody mediated but rather a type of cell-mediated response. CD8+ cytotoxic T cells and CD4+ helper T cells recognise antigen in a complex with either type 1 or 2 major histocompatibility complex. The antigen-presenting cells in this case are macrophages which secrete IL-1, which stimulates the proliferation of further CD4+ T cells. CD4+ T cells secrete IL-2 and interferon gamma, further inducing the release of other Type 1 cytokines, thus mediating the immune response. Activated CD8+ T cells destroy target cells on contact while activated macrophages produce hydrolytic enzymes and, on presentation with certain intracellular pathogens, transform
into multinucleated giant cells. Delayed hypersensitivity reactions can occur in response to protein antigens from insect bites, in transplantation reactions and also lead to skin lesions observed in smallpox and measles (Yalew,2020).
Type 5 hypersensitivity are mediated by antibodies and lead to parts of the body to malfunction (Milan, 2013) as a result of these antibodies interacting with receptors on a cell that are normally stimulated by hormones (Millar, 2021) (Milan, 2013). Examples of conditions where type 5 hypersensitivities are believed to occur (Milan, 2013) include; morbus graves, myasthenia gravis (Dresser et al., 2021) and pernicious anaemia (Vaqar and Shackelford, 2022) (Milan, 2013). Other authors, however, place myasthenia gravis under the category of type 2 reactions (Justiz Vaillant, Vashisht and Zito, 2022) demonstrating a need for more research to be done on distinction between type 2 and type HS.
Paul Gray puts up a hypothesis of another possible mechanism that may be responsible for type 5 HS. People with autoreactive effector T-cells have an overblown reaction to small circulating amounts of PAMPs, DAMPs and other localized particles within tissues, leading to the initiation of damaging pro-inflammatory signals (Gray, 2009).
The Arthus reaction was discovered by Nicolas Maurice Arthus in 1903 when he repeatedly injected horse serum subcutaneously into rabbits. He found that after four injections oedema developed at the injection site causing the serum to be absorbed slowly. Further injections resulted in the development of gangrene.
Arthus reactions, although fairly rare, are reported after patients receive vaccinations against diphtheria and tetanus, where they develop a 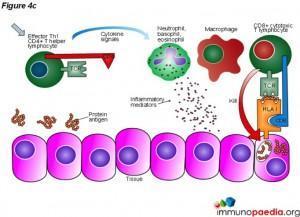 local vasculitis associated with deposition of immune complexes and activation of complement. Immune complexes form in the setting of high local concentration of vaccine antigens and high circulating antibody concentration. These reactions are characterised by severe pain, swelling, induration, edema, hemorrhage, and occasionally necrosis. This is a form of local type III hypersensitivity reaction occurring in a previously sensitized person, with signs and symptoms typically occurring 4–12 hours after vaccination.
local vasculitis associated with deposition of immune complexes and activation of complement. Immune complexes form in the setting of high local concentration of vaccine antigens and high circulating antibody concentration. These reactions are characterised by severe pain, swelling, induration, edema, hemorrhage, and occasionally necrosis. This is a form of local type III hypersensitivity reaction occurring in a previously sensitized person, with signs and symptoms typically occurring 4–12 hours after vaccination.
Download images for this case
Treatment
A dose of acetaminophen was given every 4 hours for 24 hours for pain and the child was observed at home. No further interventions were required.
Download images for this case
Final Outcome
Fever defervesced within 12 hours. Limb oedema and tenderness resolved gradually over the following two days, and the child resumed increasingly full use of the affected limb as the other clinical signs resolved. Within a week she had made a full recovery.
Download images for this case
References
Riedl MA, Casillas AM. (2003) Adverse drug reactions: types and treatment options. Am Fam Physician. Nov 1;68(9):1781-90.
Kobayashi K, Kaneda K, Kasama T. (2001) Immunopathogenesis of delayed-type hypersensitivity. Microsc Res Tech. May 15;53(4):241-5.
Siegrist CA. (2007) Mechanisms underlying adverse reactions to vaccines. J Comp Pathol. Jul;137 Suppl 1:S46-50.
Millar, H. (2021) What are the different types of hypersensitivity reactions?, Medicalnewstoday.com. Available at: https://www.medicalnewstoday.com/articles/hypersensitivity-reactions (Accessed: March 9, 2023).
Milan Buc: Hypersensitivity reactions, types II till V. Multimedia support in the education of clinical and health care disciplines :: Portal of Faculty of Medicine, Comenius University [online] , [cit. 09. 03. 2023]. Available from WWW: https://portal.fmed.uniba.sk/articles.php?aid=227. ISSN 1337-9577.
Vaqar, S. and Shackelford, K. (2022) Pernicious Anemia. StatPearls Publishing.
Yalew ST. Hypersensitivity Reaction: Review. Int J Vet Sci Technol. 2020;4(1): 028-032
Gray, P. E. A. (2009) “A 5th type of hypersensitivity reaction: does incidental recruitment of autoreactive effector memory T-cells in response to minute amounts of PAMPs or DAMPs, underlie inflammatory episodes in the seronegative arthropathies and acute anterior uveitis?,” Medical hypotheses, 73(3), pp. 284–291.
Persaud, Y., Memon, R. J. and Savliwala, M. N. (2022) Allergy Immunotherapy. StatPearls Publishing.
Justiz Vaillant, A. A., Vashisht, R. and Zito, P. M. (2022) Immediate hypersensitivity reactions. StatPearls Publishing.
Dresser, L. et al. (2021) “Myasthenia gravis: Epidemiology, pathophysiology and clinical manifestations,” Journal of clinical medicine, 10(11), p. 2235.
Download images for this case
Evaluation – Questions & answers
What is the diagnosis of this case?
How many kinds of hypersensitivity are generally recognised?
Type 1 – Immediate (also called atopic or anaphylactic)
Type 2 – Antibody-dependent
Type 3 – Immune complex
Type 4 – Cell-mediated (also called Delayed-Type Hypersensitivity, DTH)
Type 5 – Stimulatory
This is more typically a subclassification for the Type 2 reaction however some British based texts mention it as it’s own type.
What are the basic principles of the reactions and give some clinical examples?
Type 1 – immediate (or atopic, or anaphylactic)
Type 1 hypersensitivity is an allergic reaction provoked by reexposure to a specific type of antigen referred to as an allergen. Exposure may be by ingestion, inhalation, injection, or direct contact. The difference between a normal immune response and a type I hypersensitivity response is that plasma cells secrete IgE. This class of antibodies binds to Fc receptors on the surface of tissue mast cells and blood basophils. Mast cells and basophils coated by IgE are “sensitised.” Later exposure to the same allergen, cross-links the bound IgE on sensitised cells resulting in degranulation and the secretion of pharmacologically active mediators such as histamine, leukotriene, and prostaglandin that act on the surrounding tissues. The principal effects of these products are vasodilation and smooth-muscle contraction.
The reaction may be either local or systemic. Symptoms vary from mild irritation to sudden death from anaphylactic shock. Treatment usually involves epinephrine, antihistamines, and corticosteroids.
Some examples:
- Allergic asthma
- Allergic conjunctivitis
- Allergic rhinitis (“hay fever”)
- Anaphylaxis
- Angioedema
- Atopic dermatitis (eczema)
- Urticaria (hives)
- Eosinophilia
Type 2 – antibody-dependent
In type 2 hypersensitivity, the antibodies produced by the immune response bind to antigens on the patient’s own cell surfaces. The antigens recognised in this way may either be intrinsic (“self” antigen, innately part of the patient’s cells) or extrinsic (absorbed onto the cells during exposure to some foreign antigen, possibly as part of infection with a pathogen). These cells are recognised by macrophages or dendritic cells which act as antigen presenting cells, this causes a B cell response where antibodies are produced against the foreign antigen. An example here is the reaction to penicillin where the drug can bind to red blood cells causing them to be recognised as different, B cell proliferation will take place and antibodies to the drug are produced. IgG and IgM antibodies bind to these antigens to form complexes that activate the classical pathway of complement activation for eliminating cells presenting foreign antigens (which are usually, but not in this case, pathogens). That is, mediators of acute inflammation are generated at the site and membrane attack complexes cause cell lysis and death. The reaction takes hours to a day.
Another form of type 2 hypersensitivity is called Antibody Dependent Cell Mediated Cytotoxicity (ADCC). Here, cells exhibiting the foreign antigen are tagged with antibodies (IgG or IgM). These tagged cells are then recognised by Natural Killer (NK) cells and macrophages (recognised via IgG bound to the cell surface receptor, CD16 (FcγRIII)), which in turn kill these tagged cells.
See type 5 hypersensitivity reaction below, as it is sometimes used as a distinction from type 2.
Some examples:
- Autoimmune hemolytic anemia
- Goodpasture’s syndrome
- Erythroblastosis Fetalis
- Pemphigus
- Pernicious anemia (if autoimmune)
- Immune thrombocytopenia
- Transfusion reactions
- Hashimoto’s thyroiditis
- Graves’ disease
- Myasthenia gravis
- Rheumatic fever
- Hemolytic disease of the newborn
Type 3 – immune complex
In type 3 hypersensitivity, soluble immune complexes (aggregations of antigens and IgG and IgM antibodies) form in the blood and are deposited in various tissues (typically the skin, kidney and joints) where they may trigger an immune response according to the classical pathway of complement activation (see above). There are two stages relating to the development of the complexes, firstly the complex forms when IgG and IgM antibodies are bound to an antigen, after this, the complexes can form larger ones which can be cleared by the body. It is at the first stage of this formation where clearance is not possible and the antigen-antibody complex will spread and deposit as stated above. The reaction takes hours to days to develop.
Some examples:
- Immune complex glomerulonephritis
- Rheumatoid arthritis
- Serum sickness
- Subacute bacterial endocarditis
- Symptoms of malaria
- Systemic lupus erythematosus
- Arthus reaction
- Farmer’s Lung (Arthus-type reaction)
Type 4 – cell-mediated (Delayed-Type Hypersensitivity, DTH)
Type 4 hypersensitivity is often called delayed type as the reaction takes two to three days to develop. Unlike the other types, it is not antibody mediated but rather is a type of cell-mediated response. CD8+ cytotoxic T cells and CD4+ helper T cells recognise antigen in a complex with either type 1 or 2 major histocompatibility complex. The antigen-presenting cells in this case are macrophages which secrete IL-1, which stimulates the proliferation of further CD4+ T cells. CD4+ T cells cells secrete IL-2 and interferon gamma, further inducing the release of other Type 1 cytokines, thus mediating the immune response. Activated CD8+ T cells destroy target cells on contact while activated macrophages produce hydrolytic enzymes and, on presentation with certain intracellular pathogens, transform into multinucleated giant cells.
Some examples:
- Contact dermatitis (poison ivy rash, for example)
- Temporal arteritis
- Symptoms of leprosy
- Symptoms of tuberculosis
- Transplant rejection
- Coeliac disease
Type 5 – stimulatory
This type of hypersensitivity reaction is sometimes used as a distinction from Type 2 reaction.
These reactions occur when IgG class antibodies directed towards cell surface antigens have a stimulating effect on their target. Instead of binding to cell surface components, the antibodies recognise and bind to the cell surface receptors, which either prevents the intended ligand binding with the receptor or mimics the effects of the ligand, thus impairing cell signalling.
Some clinical examples:
- Graves’ disease
- Myasthenia gravis
What is the pathophysiological basis of this presumed type III hypersensitivity reaction?
What could be done to further investigate the reaction?
FBC with differential and erythrocyte sedimentation rate (ESR)
Ultra Sound – examinations to rule out localized abscess formation.
Tetanus and Pertussis antibody titres -. Elevated postvaccination titres can help to confirm diagnosis. (Prevaccination titres are of greater value, however there is no way to predict which children may be at risk and routine testing would be too expensive.)
What might be learned from this reaction that might inform the location for administration of booster doses?
What might you advise the parents regarding further boosters?
Download images for this case
Multiple Choice Questions
Earn 1 HPCSA or 0.25 SACNASP CPD Points – Online Quiz
Download images for this case
Mike Gold, The University of Adelaide – Vaccine Safety/Adverse Events