Coeliac disease is an autoimmune disorder where ingestion of gluten damages the small intestine. While most patients improve with diet modification, ~1% develop refractory coeliac disease, which does not respond to dietary control and carries a higher risk of intestinal lymphoma.
- Type 2 RCD is linked to malignant immune cells.
- Type 1 RCD was previously unexplained—this study now identifies immune cell mutations as the likely driver.
New research has uncovered why a subset of coeliac disease patients continue to suffer debilitating symptoms despite adhering strictly to a gluten-free diet (Figure 1). The study reveals that genetically mutated immune cells—undetectable by traditional methods—may be driving ongoing inflammation in the gut, offering a potential breakthrough in diagnosing and treating refractory coeliac disease.
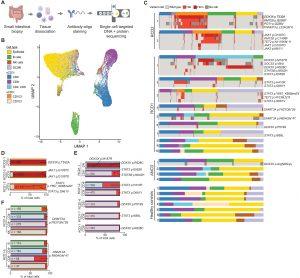
Figure 1: Single cells with somatic mutations accumulate in intestinal lymphocytes of people with RCD. (A) Experimental strategy. (B) UMAP plot of 47,946 duodenal biopsy cells analyzed for surface proteins, pooled from 23 individuals and annotated by cell type: 15,032 epithelial cells, 5252 B cells, 7645 sCD3+ CD8+ cells, 6912 sCD3+ CD4+ cells, 3263 sCD3+ CD4− CD8− cells, 798 sCD3− CD103+ cells, 963 sCD3− CD103− cells, 2174 NK cells, and 5589 DCs and macrophages (DC/Mf). (C) Box plots of 1841 cells from 2 individuals with RCD2 (patient identifier on the left), 20,894 cells from 10 individuals with RCD1, 8402 cells from 4 individuals with ANCD, and 16,809 cells from 7 healthy controls, with colored segments denoting cells assigned to the indicated cell types [per key in (B)], and the DNA somatic mutation variant calls for each cell in rows below colored as per the key. (D to F) Frequencies of cells with the indicated mutations within sCD3− CD103+ cells (D) or sCD3+ cells (E) or found in multiple cell types (F). Variant and cell type colors correspond to keys in (B) and (C). DN, CD4− CD8−; B, B cells.
- Using single-cell sequencing, scientists identified mutated immune cell clones in the intestines of patients with type 1 refractory coeliac disease—a condition where symptoms persist even after gluten elimination.
- These “rogue” immune cells carry mutations in pathways associated with immune overactivation and cancer, particularly the JAK-STAT signaling pathway.
- These findings mark the first molecular signature of type 1 refractory coeliac disease, previously a clinical mystery.
The team found that 7 out of 10 patients with type 1 RCD had immune cells with mutations commonly seen in cancers—particularly in the JAK-STAT pathway.
Further clinical trials will assess JAK inhibitors and other targeted therapies in patients with refractory coeliac disease. This approach may also help identify at-risk individuals earlier, enabling more proactive intervention.
Journal article: Singh, M., et al., 2025. Expanded T cell clones with lymphoma driver somatic mutations accumulate in refractory celiac disease. Science Translational Medicine.
Summary by Stefan Botha










