Coronavirus disease 2019 (COVID-19) is associated with severe cytokine storm, neutrophilia and increased formation of neutrophil extracellular traps (NETs). During severe infection this may lead to prominent multi-organ dysfunctions known as sepsis. It is known that hypercytokinemia in sepsis leads to the breakdown of intestinal tight junctions, allowing the translocation of e.g. lipopolysaccharide (LPS) and (1-3)-β-D-glucan (BG) from the gut into the blood circulation. Since LPS and BG are the cell wall components of gram-negative bacteria and fungi, respectively, these facilitate inflammatory responses including the formation of NETs (READ MORE).
A gut barrier defect (leaky gut) was already implicated in COVID-19, even without bacterial infection, but data on this topic is still scarce. Saithong and colleagues hypothesized now that severe COVID-19 causes leaky gut and gut translocation of pathogenic cell wall components enhancing the formation of NETs and sepsis severity (Figure 1). Therefore, the authors evaluated several clinical parameters (serum cytokine levels, serum LPS and BG, serum NET parameters like dsDNA, MPO-DNA complexes and neutrophil elastase, serum bacteria-free DNA) of patients with different disease severity. Furthermore, they analyzed the blood bacteriome and stimulated isolated neutrophils with patient-derived serum or LPS, with or without BG, and assessed NET formation.
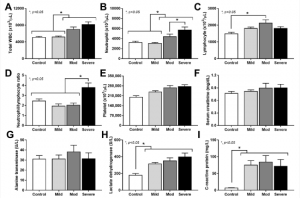
Figure 1: Characteristics of patients with COVID-19 in different severities—mild (n = 27), moderate (n = 28), and severe (n = 20), versus healthy control (n = 15), as indicated by total peripheral white blood cell count (WBC) (A), blood neutrophils and lymphocytes (B,C), neutrophil/lymphocyte ratio (D), platelet count (E), serum creatinine (F), alanine transaminase (ALT) (G), lactate dehydrogenase (LDH) (H), and C-reactive protein (CRP) (I)—are demonstrated. *—p < 0.05 between the indicated groups as determined by ANOVA with Tukey’s analysis (Saithong, et al., 2022).
Saithong and colleagues described differences in conventional blood parameters in between the different COVID-19 severities. Patients with severe COVID-19 harbored the highest blood neutrophil counts and neutrophil/lymphocyte ratio. Also, the levels of the serum cytokines TNF‑α, IL-1β, IL-6 and IL-8 were highest in this group. Since they did not detect bacteria-free DNA in the samples of patients with mild COVID-19, they only performed blood bacteriome analysis for patients with moderate and severe COVID-19. Interestingly, they found indirect evidence for gut translocation also in healthy controls since the bacteriome analysis revealed the presence of proteobacteria in the blood of healthy controls and patients with moderate to severe COVID-19. As the abundance of E. coli DNA was higher in the blood of severe COVID-19 cases, the authors concluded that a more prominent gut translocation of bacteria-free DNA takes place in severe cases compared to moderate ones. Lastly, the authors found that serum from patients with severe COVID-19 induced NETs most prominently compared to serum from healthy controls or mild to moderate COVID-19 infection.
Journal article: Journal article: Saithong, S., et al., 2022. Neutrophil Extracellular Traps in Severe SARS-CoV-2 Infection: A Possible Impact of LPS and (1→3)-β-D-glucan in Blood from Gut Translocation. Cells.
Summary by Dr. Jasmin Knopf










