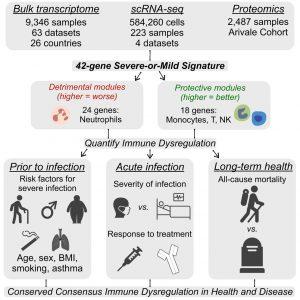
Why do some people get dangerously ill from infections while others recover quickly? Age, sex, smoking, and obesity have long been known to raise risk, but what connects these seemingly unrelated factors? In a new study researchers have uncovered a shared biological thread: a gene signature of immune dysregulation that can predict how severely a person will respond to infection even before they get sick (Figure 1).
The team analysed large-scale public datasets which contains genetic and health data from over 5,000 adults. They identified a consistent pattern in the expression of 42 immune-related genes that reveals whether a person’s immune system is well-regulated or dysregulated.
This “immune health signature” isn’t limited to COVID-19. It predicts outcomes in bacterial sepsis, asthma, and burns, showing that it reflects a person’s overall immune resilience rather than a response to a single pathogen.
People with higher scores for immune dysregulation, particularly older adults, men, smokers, and those with obesity or diabetes, had worse infection outcomes and a higher likelihood of dying from any cause, even without active infection. Among the 42 genes, two clusters reflect protective immune activity, while the other two amplify harmful inflammation. The balance between these “good” and “bad” arms of the immune system appears to determine immune health.
Genes linked to neutrophils, white blood cells that can suppress other immune cells when overactive, were associated with poor outcomes. In contrast, genes tied to T cells, monocytes, and natural killer (NK) cells correlated with healthier, more balanced immune responses.
Encouragingly, the study found that immune dysregulation is not fixed.
• Former smokers who had quit for over five years showed improved immune health compared to current smokers.
• People with diabetes who controlled their blood sugar had healthier immune signatures than those with poorly managed diabetes.
• In another study, calorie restriction in overweight individuals reduced immune dysregulation compared to those maintaining regular diets.
These findings suggest that lifestyle changes – quitting smoking, improving diet, or managing chronic conditions, can help restore immune balance at the molecular level.
The ability to measure immune health could transform medicine. Just as cholesterol levels help gauge cardiovascular risk, this immune gene signature might one day serve as a biomarker for immune fitness, allowing doctors to identify people at risk before illness strikes and guide personalized prevention strategies.
The researchers have identified a molecular fingerprint of immune health that predicts disease severity across infections and conditions and can be improved through lifestyle changes. It’s a step toward a future where immune fitness can be measured, monitored, and optimized.
Journal article: Ganesan, A., et al. 2025. A conserved immune dysregulation signature is associated with infection severity, risk factors prior to infection, and treatment response. Immunity.
Summary by Stefan Botha