In a recent study, researchers have made a significant discovery about memory CD4+ T lymphocytes, crucial players in our immune response, in the context of HIV infection (Figure 1). Building on previous research in mice that demonstrated how chronic inflammation can lead to cell death in certain cells, the team investigated this mechanism in the context of HIV.
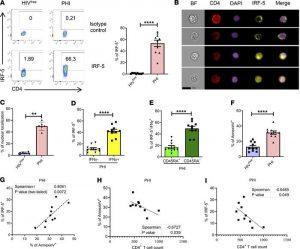
Figure 1: IRF5 is expressed in CD4+ T cells from PHI. PBMCs from PHI and HIVfree individuals were analyzed by flow cytometry. (A) Representative FACS plots and percentage of IRF-5+ CD4+ T cells. (B) Representative ImageStreamX images of CD4+ T cells expressing IRF5 in the cytoplasm (first 2 lanes) and in the nucleus (third and fourth lane). (C–F) Graphs show (C) the frequency of CD4+ T cells whose IRF-5 expression colocalizes with the nucleus; (D) the percentage of IFN-γ+ and IFN-γ–IRF-5+ CD4+ T cells; (E) the frequency of CD45RA+ and CD45RA–IFN-γ+ CD4+ T cells expressing IRF-5 in PHI individuals; and (F) the percentage of annexin V+CD4+ T cells from PHI and HIVfree individuals. Data are presented as the mean ± SD. The Mann-Whitney U test was used for significance. **P < 0.01, ****P < 0.0001, n =10. Graphs represent correlations between (G) annexin V and IRF-5 expression in CD4+ T cells, (H) annexin V expression and CD4+ T cell count, and (I) IRF-5 expression and CD4+ T cell count in PHI donors. The Spearman’s r test was used for significance, *P < 0.05, **P < 0.01, n =10.
Despite undergoing antiretroviral treatment, many individuals living with HIV still experiences remaining inflammation. Notably, memory CD4+ T cells in these individuals are known to be particularly susceptible to cell death. However, until now, the specific underlying mechanism behind this vulnerability remained largely unknown.
The study revealed that memory CD4+ T cells have a higher expression of two molecules: the TLR7 receptor and the IRF5 transcription factor. This increased expression creates a predisposition to cell death in these cells. Excitingly, the researchers found that this predisposition can be blocked by IRF-5 inhibitory peptides, offering a potential therapeutic approach.
These findings have significant implications not only for HIV treatment but also for other chronic infectious diseases characterized by persistent inflammation. By shedding light on the mechanism behind the vulnerability of memory CD4+ T cells, this research paves the way for the development of more targeted and effective therapies.
For individuals with HIV who do not respond well to current treatments, this breakthrough could open the door to a more suitable and tailored therapy. Furthermore, this study highlights the importance of understanding the immune response in chronic infections, which could have far-reaching implications for future therapeutic interventions.
Journal article: Carmona-Pérez, L., et al., 2023. The TLR7/IRF-5 axis sensitizes memory CD4+ T cells to Fas-mediated apoptosis during HIV-1 infection. JCI Insight.
Summary by Stefan Botha










