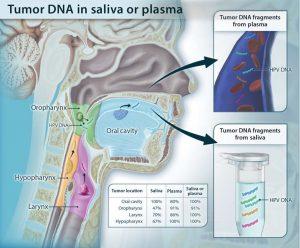
Schematic showing the shedding of tumor DNA from head and neck cancers into the saliva or plasma. Tumors from various anatomic locations shed DNA fragments containing tumor-specific mutations and HPV DNA into the saliva or the circulation. The detectability of tumor DNA in the saliva varied with anatomic location of the tumor, with the highest sensitivity for oral cavity cancers. The detectability in plasma varied much less in regard to the tumor’s anatomical location. (Source: Wang et al., 2015).
Cancers are very challenging diseases viewed from numerous aspects. For the most efficient care and survey of patients, diagnostic, prognostic theragnostic biomarkers are needed.
Hence, tumour antigens such as Prostate Specific Antigen (PSA) and Carcinoembryonic Antigen (CEA) have been proposed and validated as diagnostic biomarkers and immunoscore has been proposed as prognostic tool. However, these biomarkers may either lack sensitivity (PSA) or specificity (CEA) or they need invasive sample collects (Biopsies for immunoscore). Decades ago, it was postulated that circulating altered tumour DNA (ctDNA) is a less invasive biomarker in numerous cancers despite the technical challenges of detecting such low amounts of ctDNA in body fluids (plasma, stool, Pap smear fluids, sputum, and urine). Over the last several years, however, technological advances have made it possible to detect these biomarkers even when they occur in low amounts.
Although head and neck squamous cell carcinomas (HNSCCs) is the seventh most frequent type of cancer, they both still have no validated biomarkers and lack specific therapies. This proof of principle study by Wang and colleagues aimed, to underline the potential of ctDNA as biomarker in saliva and plasma from 93 patients with various entity of HNSSC (oral, oropharyngeal, laryngeal and hypopharyngeal).
The best sensitivity (100%) was obtained with ctDNA detection in saliva from patients with oral cavity squamous cell carcinomas at early disease stages. Similarly, a sensitivity of 96% was determined in HNSCCs when ctDNA was analysed simultaneously in plasma and saliva. Furthermore, ctDNA was able to predict relapse when it was found after surgical care. Thus, ctDNA could allow to diagnose these diseases early and consequently improve patient outcomes.
Despite the need to confirm this results in a larger study population, detection of ctDNA could become either an alternative or a complementary to an immunologic diagnostic and prognostic tools in HNSCCs and others cancers.
Journal Article: Wang et al., 2015. Detection of somatic mutations and HPV in the saliva and plasma of patients with head and neck squamous cell carcinomas. Science Translational Medicine
Summary by Doudou Georges Massar Niang










