 IUIS-ALACI-ACAAI Immuno-Colombia 2021 course took place remotely between 5th to 16th April. The theme of this meeting was “Mechanisms and Approaches to Immunotherapy for Cancer and Chronic Inflammatory Diseases”. Today, we highlight a talk by Professor Gloria Vasquez (University of Antioquia, Colombia) entitled “Anti-Cytokine Therapies”
IUIS-ALACI-ACAAI Immuno-Colombia 2021 course took place remotely between 5th to 16th April. The theme of this meeting was “Mechanisms and Approaches to Immunotherapy for Cancer and Chronic Inflammatory Diseases”. Today, we highlight a talk by Professor Gloria Vasquez (University of Antioquia, Colombia) entitled “Anti-Cytokine Therapies”
This summary highlights the lecture by Professor Gloria Vasquez (University of Antioquia, Colombia) who discussed anti-cytokine therapy as a way to manage many autoimmune and inflammatory diseases.
In the first part of her presentation, Prof. Vasquez gave a short introduction about cytokines and their important role in health (regulation of immune responses, wound healing, angiogenesis, hematopoiesis, and tissue remodelling) and disease, in particular canonical inflammation processes such as heat, redness, swelling, pain, and loss of function.
Did you know the first cytokine to be discovered was interferon (IFN) in 1957?
Inflammatory cytokines are important for immune defence. However, excessive and persistent inflammatory cytokines can cause immunopathology and result in autoimmune diseases. To demonstrate this, Prof. Vasquez gave the example of how cytokines play a role in the immunopathology of Rheumatoid Arthritis (RA), a chronic inflammatory autoimmune disease characterised by a breach of immune regulation in the joint synovial membrane leading to joint destruction. She then described the different therapeutic approaches researchers investigated to find the adequate molecule (cytokine) that plays a central role in this disease. This led to the discovery of the TNF cytokine as an effective therapeutic target to manage RA.
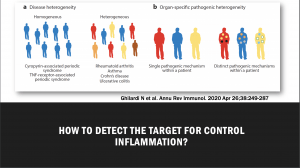
She then discussed how targeting and for manipulating cytokine regulation is a big challenge in some autoimmune and inflammatory diseases due to disease and patient heterogeneity. The use of genetic models has shown some limitations, including:
- Differences exist in disease pathogenesis during disease initiation and effector phases
- Gene-deficient organisms (humans included) can exhibit marked sensitivities to infectious challenges
- Animals housed under specific-pathogen-free conditions have immune systems that resemble that of a newborn human more than that of an antigen-experienced adult patient
- Complete inactivation of a gene may be harmful.
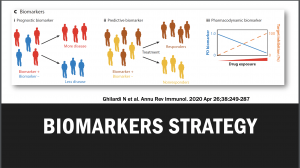
 Thus identifying disease biomarkers could lead to the development of immunotherapy that would be successful in most if not all people suffering from that specific disease. The use of predictive, prognostic, and pharmacodynamic biomarkers in drug development can at least mitigate the issues of patient heterogeneity for clinical outcome measures, and determine whether sufficient target inhibition has been achieved, respectively.
Thus identifying disease biomarkers could lead to the development of immunotherapy that would be successful in most if not all people suffering from that specific disease. The use of predictive, prognostic, and pharmacodynamic biomarkers in drug development can at least mitigate the issues of patient heterogeneity for clinical outcome measures, and determine whether sufficient target inhibition has been achieved, respectively.
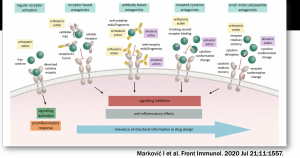
 How do you choose a cytokine as a target for immunotherapy? As described above inflammatory cytokines are essential for human health. Therefore, blocking these cytokines to prevent autoimmune diseases could increase susceptibility to other infections. Due to this, a very good understanding of the molecular mechanisms and activity of each cytokine is required to select the appropriate inflammatory target that would result in safe and efficacious immunotherapy.
How do you choose a cytokine as a target for immunotherapy? As described above inflammatory cytokines are essential for human health. Therefore, blocking these cytokines to prevent autoimmune diseases could increase susceptibility to other infections. Due to this, a very good understanding of the molecular mechanisms and activity of each cytokine is required to select the appropriate inflammatory target that would result in safe and efficacious immunotherapy.
In the next summary, we shall discuss how this is achieved and why monoclonal antibodies are excellent molecules to target cytokines in anti-cytokine therapy.
- Interested in learning more about anti-cytokine therapies: read advanced pre-course material on Anti-cytokines Therapies
- Full lecture recording available at IUIS-ALACI-ACAAI Immuno-Colombia 2021 Lecture week 1
Summary by Zeineb Zian