 “All Disease Begins in the Gut” is a famous quote attributed to Hippocrates, a physician from ancient Greece. Although our understanding of the connection between the gut and disease pathogenesis has improved considerably over the last two millenia, many questions pertaining to this topic remain unanswered. An example to this is the concept of the “gut-skin” axis implicated in the pathogenesis of certain skin disorders, such as psoriasis.
“All Disease Begins in the Gut” is a famous quote attributed to Hippocrates, a physician from ancient Greece. Although our understanding of the connection between the gut and disease pathogenesis has improved considerably over the last two millenia, many questions pertaining to this topic remain unanswered. An example to this is the concept of the “gut-skin” axis implicated in the pathogenesis of certain skin disorders, such as psoriasis.
In their recent Frontiers in Immunology article, Yegorov and colleagues (Yegorov et al.,) report that psoriasis patients have elevated levels of interleukin-1 alpha (IL-1α), a cytokine central to the control of inflammation. In addition, the researchers found that psoriais is associated with alterations of the gut microbiome, which persisted over time.
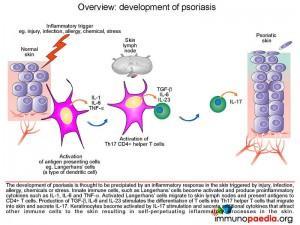
Psoriasis is a chronic autoimmune condition of the skin. The disease is debilitating and stigmatizing, and although remission is achievable in some cases, psoriasis is currently not curable. Therefore, a better understanding of the disease etiology is urgently needed to design more effective psoriasis treatment modalities. This is especially important in low-and middle-income countries (LMIC), where shortages of resources may prevent timely intervention. There is evidence that gut microenvironment may plan an important role in psoriasis pathogenesis, and if so- then modulating it using microecological agents might have a major impact on patient management.
Yegorov and co-authors conducted their study in Kazakhstan, the researchers expanded on their earlier study of the Kazakh gut microbiome and conducted a cross-sectional study to test the hypothesis that psoriasis in adults is associated with gut inflammation and microbiome alterations. Using multiplex ELISA and 16S rRNA gene sequencing they demonstrated that psoriasis is associated with elevated gut IL-1α and altered abundance of Firmicutes, supporting the notion that psoriasis is linked to gut dysbiosis and inflammation.
The results from this study are thought-provoking and intriguing, suggesting novel treatment possibilities to explore, but many questions remain to be answered. One dilemma pertains to the causality of the relationship between gut immunity and microbiota versus systemic and skin inflammation. Notably, this study is the first to characterize psoriasis in a population from Kazakhstan and to assess its associations with gut microenvironment. The authors are hopeful that this work will pave way to future studies on psoriasis in Central Asia.
Also read our case study: A case of scaly annular plaques
References
- Yegorov et al., 2020. Psoriasis Is Associated With Elevated Gut IL-1α and Intestinal Microbiome Alterations. Frontiers in Immunology
- Kushugulova et al. 2018. Metagenomic analysis of gut microbial communities from a Central Asian population. BMJ Open.
Summary by Sergey Yegorov










