New research shows that protecting infants from RSV could prevent asthma later in life.
A major international study has uncovered compelling evidence that respiratory syncytial virus (RSV) infection in early infancy sharply increases the risk of developing childhood asthma (Figure 1). The findings suggest that preventing RSV infection in newborns could dramatically reduce asthma cases, especially among children already genetically predisposed to allergies.
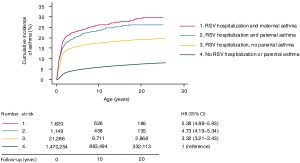
Figure 1: Cumulative incidence of asthma according to RSV hospitalization during infancy and parental asthma status. Kaplan-Meier curves showing cumulative incidence of asthma by hRSV hospitalization during infancy and parental asthma status. Cox regression models adjusting for age and sex were used to assess risk of asthma according to RSV hospitalization and parental asthma status. RSV hospitalization during infancy was admission with ICD-10 diagnoses B974, J121, J205, and J210 in the first 6 months of life. Asthma was admission with ICD-10 diagnoses J45 or J46 in 1994 to 2018. Data were collected from 1994 to 2018.
Across Europe, 5–15% of children live with asthma, a lifelong condition that impacts breathing, development, and quality of life. While genetics, environment, and immune development all contribute, the early-life triggers that push children toward asthma are still being uncovered.
This new study reveals a powerful interaction:
- Early RSV infection in the first months of life
- Inherited allergy risk, transmitted through allergen-specific antibodies from the parents
Together, these factors reshape how an infant’s immune system reacts to common allergens, in ways that increase the likelihood of asthma.
The researchers combined two powerful approaches:
- Nationwide Danish registry data, covering every child and their parents
- Controlled laboratory experiments examining infant immune responses
They found that infants who experienced severe early RSV infections were more likely to develop hypersensitive immune responses to allergens such as house dust mites. In babies with a family history of asthma or allergy, this effect became even stronger, as maternal antibodies further heightened immune reactivity.
The most hopeful finding:
When newborns were protected from RSV, the harmful immune changes did not occur, and asthma development was prevented in experimental models.
New RSV prevention tools, including maternal vaccination in late pregnancy and long-acting monoclonal antibodies for newborns, are being rolled out in many countries. Despite their proven ability to prevent severe RSV disease, uptake has been inconsistent.
This study sends a powerful message:
Preventing RSV in infancy may also prevent asthma, not just short-term infections.
Early RSV infection can prime the infant immune system toward allergy and asthma, especially in genetically at-risk children. Protecting newborns from RSV could offer one of the first truly preventive strategies against childhood asthma.
Journal reference: De Leeuw, E., et al. 2025. Maternal allergy and neonatal RSV infection synergize via FcR-mediated allergen uptake to promote the development of asthma in early life. Science Immunology.
Summary by Stefan Botha










