Children are less susceptible to SARS-CoV-2 infection and even if they do become infected, majority of children will have asymptomatic or mild COVID-19 and have a better prognosis than adults. Recent reports (predominantly from Europe & N.America) have described cases of severe hyperinflammation in children infected with COVID-19 such as Kawasaki-like disease, and have been collectively termed as Multisystem Inflammatory Syndrome in Children (MIS-C) associated COVID-19 by the WHO.
“Whether MIS-C reflects a parallel COVID-19-associated hyperinflammatory state in the pediatric population is an important question to investigate. Moreover, how the clinical and laboratory features of MIS-C relate to known syndromes of hyperinflammation and cytokine storm in children including Kawasaki Disease (KD) and macrophage activation syndrome (MAS) has not been studied in detail. In this study, Lee et al., 2020 describe 28 confirmed cases of MIS-C (n=17 of whom were admitted to the intensive care unit) at Boston Children’s Hospital and discuss the immunologic findings and management of these patients. We compare the characteristics of this novel syndrome with historic cohorts of patients with KD and MAS.” (Source Lee et al., 2020)
Lee et al., reported that “common features of MIS-C included gastrointestinal symptoms (54%), conjunctivitis (57%) and skin rash (36%)… with <50% having respiratory impairment.” Further, they showed that though some clinical features of MIS-C overlap with KD and MAS. However, MIS-C is distinct from KD and is associated with lower levels of MAS-associated molecules e.g IL-18, CXCL9 and Ferritin than MAS.
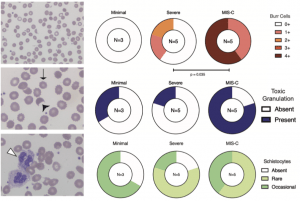
Number of patients with degree of burr cells, toxic granulation, and schistocytes for each clinical phenotype; N=13 patients with smears available. Severe COVID-19 was compared to MIS-C using Chi-squared test for trend for burr cells, Chi-squared statistic was impossible to compute for the dichotomous outcome of toxic granulation due to low N. There were no statistically significant differences in schistocytes across the cohort. (Source: Diorio et al., 2020)
Another study by Diorio et al., aimed to determine clinical and immunological features that could distinguish between severe COVID-19 and MIS-C in children. They showed that MIS-C was associated with higher expression of IL-10 & TNF compared to severe COVID-19 and COVID-19/MISC co-morbidities, while circulating IL-8 levels are higher in severe COVID-19 compared to MISC. Based on differential inflammatory cytokine expression, researchers showed that combined expression of IL-10 & TNF could potentially be used as a biomarker to distinguish the two pathological diseases. Further histology of blood samples, demonstrated that MIS-C was associated with abnormal red blood cell smears, characterised by detection of burr cells (RBC with an abnormal cell membrane that has small horny projections) and fragmented RBC with irregular non-biconcave shape.
In summary, detection of MIS-C paediatric COVID-19 presents a challenge in the clinical care of severe paediatric COVID-19, “cytokine profiling and examination of peripheral blood smears may distinguish between patients with MIS-C and severe COVID-19 only”, and could contribute to early detection and improved management of MIS-C associated COVID-19.
Journal Articles:
- Diorio et al., 2020. Multisystem inflammatory syndrome in children and COVID-19 are distinct presentations of SARS-CoV-2. JCI
- Lee et al., 2020. Distinct clinical and immunological features of SARS-COV-2- induced multisystem inflammatory syndrome in children. JCI
Summary by Cheleka Mpande










