In a recent study, scientists used machine learning to create a unique COVID-19 vaccine that targets the stimulation of T cells and is intended to be a pan-variant vaccine (Figure 1).
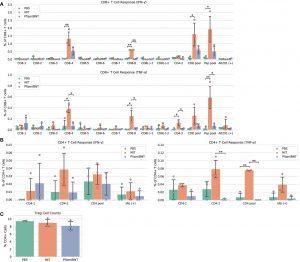
Figure 1: Vaccine immunogenicity. (A) CD8+ T cell responses, (B) CD4+ T cell responses, (C) Foxp3+ regulatory T cells (Tregs) as a percentage of all CD4+ cells. The CD8 pool includes MHC class I peptides CD8-1—CD8-8 (Supplementary Table 1). The CD4 pool includes MHC class II peptides CD4-1 and CD4-2. The Pep pool includes all query peptides in Supplementary Table 1 except CD4-3. Error bars indicate the standard deviation around each mean. P values were computed by one-way ANOVA with Tukey’s test. *P < 0.05, **P < 0.01.
For every viral strain—be it alpha, beta, delta, or omicron—for which researchers believed they had effectively developed a vaccine, another variant or subvariant soon followed. By exposing the immune system to a tiny portion of the virus, viral vaccines usually function. When individuals are exposed to the real virus afterward, those learned reactions can safeguard them. Standard COVID-19 vaccines, like those made by Moderna and Pfizer, work by stimulating the immune system’s production of blocking antibodies.
By choosing a new target for their vaccine—activating the immune system’s “killer” T cells, which attack virus-infected cells—the researchers in this study took a different strategy to normal vaccine creation pipelines. Although a COVID-19 vaccine won’t prevent people from acquiring the disease, it might prevent them from becoming seriously unwell or even dying.
A challenging collection of optimization issues was resolved using machine learning techniques. The main objective is to choose peptides that are present, or “conserved,” in all viral types. But for those peptides to warn the immune system, they also need to be linked to human leukocyte antigens (HLA) molecules that have a high chance of being expressed.
Before this study can bring in these novel vaccines, more animal studies—and eventually human studies—must be conducted. According to the researchers, immunocompromised people who are unable to make neutralizing antibodies and may not profit from conventional COVID vaccines may be helped by this novel T-cell vaccine. Their vaccine may also lessen the symptoms of “long COVID” in those who retain viral reservoirs long after their original exposure.
Journal article: Brandon Carter., B. et al., 2023. A pan-variant mRNA-LNP T cell vaccine protects HLA transgenic mice from mortality after infection with SARS-CoV-2 Beta. Frontiers in Immunology.
Summary by Stefan Botha










