Our brains can trigger immune defences at the mere sight of someone who appears sick, even without direct exposure to pathogens. A new study demonstrates that visual cues of illness are enough to activate front-line immune cells, revealing a powerful link between perception and immunity (Figure 1).
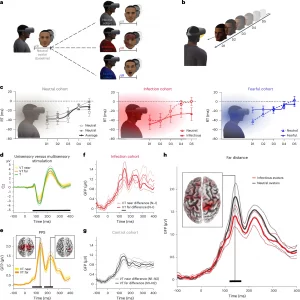
Figure 1: Early detection of infectious avatars by the PPS system. a, VR setup. Participants were first exposed to a neutral avatar (baseline) and then assigned to one of three cohorts encountering neutral, infectious or fearful avatars in a second session. b, PPS task. Participants responded to tactile stimuli on their face, delivered either in empty space (unisensory) or combined with an avatar approaching (multisensory). Tactile stimuli (flash icon) were presented at five delays, with the avatar located at one of five distances (D5 = far, D1 = near). c, PPS representation across cohorts. Reaction times (RTs) to multisensory stimuli were normalized by unisensory RTs (dotted line) and plotted by avatar distance. Shaded areas illustrate the PPS gradient, defined by significantly faster multisensory RTs (P < 0.05, corrected; paired-sample t-tests); N = 15 per cohort. Data are shown as mean ± s.e.m. (see Supplementary Table 3 for full statistics). d–h, EEG responses recorded from the central electrode (Cz) as an example (N = 16 per cohort). Black segments denote statistically significant time windows (cluster-based, nonparametric statistical tests; P < 0.01, corrected; solid lines = mean EEG response; dotted lines = 95% confidence interval). d, Evoked responses comparing unisensory (T) and multisensory (VT) stimulation as an index of multisensory processing. e, GFP analysis of PPS-related processing, that is, VT response differences for near versus far avatars. Insets show near–far current distribution differences at peak GFP effects. f, Significant GFP difference for near versus far stimulation between infectious and neutral avatars in the infection cohort. g, No GFP differences were found between two neutral avatars in the control cohort. h, Significant GFP differences between infectious and neutral avatars at the far location in the infection cohort, with the inset showing peak current distribution difference.
Researchers used virtual reality (VR) headsets to immerse healthy volunteers in social encounters with human avatars. Some avatars displayed symptoms such as coughing or rashes, while controls appeared healthy. As avatars approached, brain imaging revealed activation of regions involved in personal-space monitoring and the salience network, circuits that detect and prioritize threats. This suggested that the brain anticipates possible infection risk and mounts pre-emptive responses.
Critically, the team showed that this proactive neural anticipation does more than alter perception: it drives immune change. Potential contact with “infectious” avatars entering the peripersonal space, the immediate zone surrounding the body, activated multisensory–motor areas and the salience network, as measured with psychophysics, electroencephalography (EEG), and functional MRI. This brain activity instigated measurable immune effects, including changes in both the frequency and activation of innate lymphoid cells, key first-line defenders against pathogens. These immune shifts closely mirrored those seen in participants exposed to an influenza vaccine, underscoring the parallels between perceived and actual infection.
Further analysis revealed that altered connectivity between infection-sensing brain regions and the hypothalamus, along with modulation of neural mediators, linked these responses to the hypothalamic–pituitary–adrenal (HPA) axis. Neural network modelling supported this integrated neuro–immune crosstalk, showing how anticipation of infection alone can coordinate brain and immune responses.
Beyond advancing basic understanding, the work carries translational potential. The authors propose that VR-based strategies might one day be harnessed to enhance vaccine efficacy by boosting immune readiness.
Trabanelli, S. et al. 2025. Neural anticipation of virtual infection triggers an immune response. Nature Neurosci.
Summary by Stefan Botha










