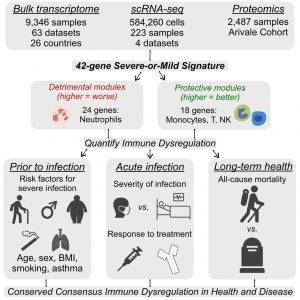
In a new study, researchers have shown that a 42-gene “Signature of Misfiring” (SoM) serves as a robust predictor of immune dysfunction across individuals at high risk of severe infections (Figure 1).
Conducting a large-scale analysis of 12,026 blood samples, the team extended the SoM signature, initially discovered in COVID-19 patients, to a broader population, including older adults, males, individuals with obesity, and those with comorbidities. Remarkably, this signature remained consistently detectable among these high-risk groups, even before infection occurred.
Key Findings:
- Conserved Across Risk Groups: The SoM signature reliably indicates immune dysregulation tied to demographic and health-related risk factors.
- Predictive of Clinical Outcomes: Individuals with elevated SoM scores were more likely to benefit from corticosteroid treatments and showed higher all-cause mortality.
- Implications for Early Intervention: Detecting misregulated immune states before illness could enable clinicians to:
- Identify individuals most likely to benefit from steroid therapy.
- Initiate targeted treatment earlier, potentially reducing the severity of eventual infections.
This signature reflects a consistent molecular pattern that links demographic risk factors to underlying immune dysfunction, offering a pathway toward personalised pre-emptive care.Instead of relying solely on observable symptoms or conventional biomarkers, using a molecular signature like this could revolutionise how we:
- Risk-stratify patients before infection.
- Tailor preventive therapies, such as corticosteroids, based on individual immune profiles.
- Enhance patient outcomes, potentially reducing hospitalizations and mortality.
By combining high-throughput transcriptomics with real-world clinical data, this research lays the foundation for a proactive approach to infectious disease, one driven by molecular insight rather than reactive treatment.
Journal article: Ganesan , A., et al. 2025. A conserved immune dysregulation signature is associated with infection severity, risk factors prior to infection, and treatment response. Immunity.
Summary by Stefan Botha