Immunopaedia attended the Beyond Sciences Initiative 2nd Annual Remote Conference: Science and Society from 28-29 Janaury, 2017. This week we will be highlighting some of the interesting presentations from the conference.
Dr Thumbi Ndung’u from the Kwazulu-Natal Research Institute for TB-HIV, South Africa shared his current findings in using highly active antiretroviral therapy (HAART) to suppress viraemia in HIV acutely-infected individuals in their South African cohort.
One of the big questions in HIV research is whether there is a need to find a cure given the current preventative measures and treatment options available. For example, improved drug regimens such as HAART have enabled HIV infected individuals to live long and healthy lives; so why the need for a cure?
Even though drugs are effective, they do cause adverse side effects. HIV treatment has been associated with cardiovascular and renal diseases as well as malignancies and bone disorders to name a few. The drugs need to be taken for the rest of the infected person’s life leading to adherence and drug resistance problems. Therefore, even though there are many treatment options currently available, an HIV cure is still important.
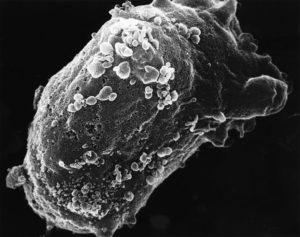
One of the barriers to curing HIV is that the virus enters cells and hides there in a latent state. Another problem is that the virus does not become completely suppressed and continues to replicate even with treatment.
One strategy to overcome this is to treat HIV infected individuals with HAART in the hyperacute phase of infection before peak viraemia is reached. This is the strategy that the researchers led by Thumbi Ndung’u took.
The team recruited women between the ages of 18-23 years old. These women were all at high risk of HIV acquisition and visited the clinic twice a week to provide blood samples to be tested for the presence of HIV RNA. The study went on for one year.
As of June 2016, 42 participants tested positive for HIV. 28 participants were provided HAART at the hyperacute stage of infection while 14 were untreated as per the current World Health Organization guidelines. They found that the treated women had no dips in CD4 count during acute infection and their viraemia did not increase substantially over the time period they were followed. These observations were not seen in the untreated arm.
Most of the treated participants did not seroconvert throughout the duration of the study. The treated group made less HIV-specific CD8 cells. Although the quantity was lower, the treated group made more functionally competent CD8 responses.
This study sheds light on long term remission and how the use of early ART may be able to suppress viral replication and lead to a functional cure to HIV. The study is also useful in understanding treatment interventions and their impact on the immune system.
For more information on the conference visit: 2nd Annual International Remote Conference: Science and Society
Article by Thandeka Moyo