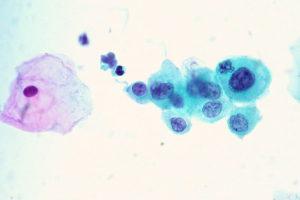
Human papillomavirus (HPV) is the most common sexually transmitted virus with up to 80% of the sexually active population becoming infected at one point in their lifetime. HPV contributes to the mortality and morbidity of populations, where prevention is scarce and infection can sometimes lead to HPV-associated cancers including cervical cancer. Viruses including HPV have the ability to manipulate host gene expression to avoid immune response by the host. It has been found that HPV oncoprotein E7 interacts with DNA methyltransferase 1, an epigenetic enzyme responsible for transferring methyl donors to DNA. Researchers have been investigating possible epigenetic effects of HPV since it the potential to regulate genes associated with tumour suppression and immunity. Keratinocytes, cells of the epidermis, are purported target cells of HPV. Colorado researchers investigated DNA methylation in keratinocytes to classify mechanisms influenced by HPV using global gene expression and methylation analysis.
Cicchini et al. observed that many strongly upregulated genes by high-risk HPV in keratinocytes were associated with cell cycle functions, notably DNA replication. Distant cell cycle-associated genes were also investigated to evaluate physiological relevance. When comparing HPV-positive cancers to HPV-negative controls, HPV-positive cancers had more upregulated cell cycle genes. Specifically assessing oncoprotein E7, affected genes were also associated with DNA repair by upregulation. Contrarily, non-E7-mediated genes were downregulated and involved with IL-1 signalling, extracellular matrix degradation, and antigen presentation. Furthermore, it was reported that E7-dependent methylation causes the downregulation of CXCL14, a modulator of immunity and inflammation. Overall, immune response signalling cascades were some of the most affected pathways by E7 expression. This suggests that high-risk HPV16 E7 through epigenetic modification affects antitumor immune responses. It should be noted that researchers remarked that HPV16 epigenetic modification likely differs from HPV18.
Majorhistocompatibility complex class 1 (MHC-I) and human leukocyte antigen E (HLA-E) molecules were downregulated by E7 mediation. However, HLA-E was only affected by high-risk HPV, whereas low-risk HPV did not sufficiently downregulate the protein expression. These molecules are immunologically significant since HLA-E encodes for MHC subunit proteins and regulates NK and CD8+ T cells.
High-risk HPV E7 protein is associated with affecting antiviral immunity through its downregulation of HLA-E. Furthermore, researchers were able to categorize global gene expression on numerous keratinocyte cell lines, creating a better understanding of the interaction between HPV, cell cycle genes, and immune response.
Article by Rebecca Ng