Obesity -a risk factor for allergic and autoimmune diseases in children- is hypothesised to contribute to low levels of chronic inflammation with increased lymphocyte infiltration in adipose tissue. The exact mechanism of this immunopathology is relatively unknown.
Th17 cells, a CD4+ T helper phenotype characterised by expression of RORC, transcription factor, and production of IL-17 cytokine, are important for clearance of pathogens such as fungi, as well as play a role in autoimmune and allergic inflammation. Studies of obesity in mouse models have illustrated that Th17 cells contribute to sustained chronic inflammation in these mice. Elevated levels of Th17 cells have been observed in the spleen and adipose tissue of obese mice compared to normal weight mice, further suggesting a role in chronic inflammation. Additionally, studies have shown an increased proportion of Th17 cells in peripheral blood from children with obesity and diabetes mellitus. However, these studies did not control for potential co-morbidities with chronic inflammatory and/or autoimmune diseases, conditions typically associated with increased Th17 T cell function.
To determine if obesity in children is associated with elevated Th17 cells. Schindler et al. studied Th17 cell function in normal weight (n=50) and overweight (n=15) children with no evidence of asthma, atopic dermatitis, allergic rhinoconjunctivitis, autoimmune diseases and infection 2 weeks prior to enrolment. Schindler et al. detected Th17 cell function by performing non-specific (Ionomycin) stimulation of peripheral blood mononuclear cells followed by detection of IL-17A production by CD4+(CD3+) T cells using flow cytometry, and detection of RORC and IL-17A mRNA using real-time PCR.
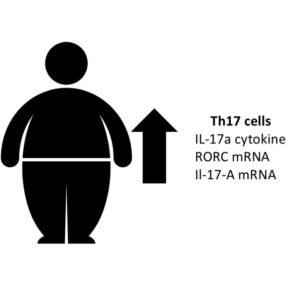
Schindler et al. observed significantly higher frequency of Th17 cells and increased mRNA expression of RORC and IL-17A in overweight children compared to non-overweight children. Interestingly, they did not observe a linear correlation between BMI and frequency of Th17 cells in the children they studied, an observation they attributed to low sample size.
In summary, Schindler et al. demonstrated an elevated Th17 cell function in overweight children in the absence of chronic inflammatory disease or infection, which might contribute to a state of increased pro-inflammation in overweight children.
Journal Article: Schindler et al. 2017. Th17 cell Frequency in Peripheral Blood is elevated in Overweight children without chronic inflammatory Diseases. Frontiers in Immunology.
Article by Cheleka AM Mpande