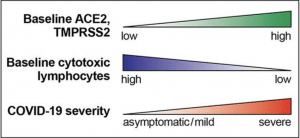
Individuals with high baseline levels of ACE2 and TMPRSS2 show low baseline tissue-resident levels of cytotoxic lymphocytes in the lung. I propose that this may jointly predispose these individuals to development of severe COVID-19. (Source: Duijf 2020)
In a journal published by the American Society of Microbiology, cancer biology researcher Pascal Duijf outlined how differences in expression within lung tissue may impact the effect of SARS-CoV-2 infection on the individual. It has been established that SARS-CoV-2 is more infectious and efficient when located in human lung tissue in comparison to its counterpart, SARS-CoV-1, or SARS. Patients with severe COVID-19 infection present with the most intense symptoms in the lungs. This may be tied to direct upregulation of the SARS-CoV-2 entry receptor, angiotensin-converting enzyme 2 (ACE2). Regarding the cellular immune response, several types of leukocytes have been associated with viral detection and response to SARS-CoV-2 infection. CD4+ and CD8+ T-cells, NK cells, dendritic cells, M1 macrophages, and neutrophils have all been studied as mediators within viral lung infections. Specifically, the cytotoxicity of CD8+ T-cells and NK cells can contribute to viral clearing and prevention of systemic dissemination.
This study evaluated levels of various cytotoxic and immune cells, as well as a number of cytokines that attract these cells, in the context of human lung tissue. ACE2 expression and levels of CD8+ T-cells, NK cells, and M1 macrophages were negatively correlated. Both resting and activated NK cells were negatively correlated. Baseline levels of cytokines CCL2 to CCL5, CXCL9, CXCL10, CXCL16, and IL-6, known chemotactic attractants of cytotoxic T-cells and NK cells, were found to be significantly correlated with the baseline levels of cytotoxic T-cells and NK cells. Conversely, several of these cytokines were found to be negatively correlated with ACE2 levels. There was no significant correlation of ACE2 expression with CD4+ T-cells, dendritic cells, and neutrophils. This led to the conclusion that ACE2 expression is associated with cytotoxicity. Immunohistochemistry also indicated that there is a strong ACE2 mRNA-protein correlation in 40 human tissues. This correlation was ranked in the top 2 percentile of the strongest 12000 mRNA-protein level correlated genes.
Specific to COVID-19, SARS-CoV-2 infection was associated with upregulation of the aforementioned cytokines in human lung cells. This was also found in lung tissues from COVID-19 patients with the majority of the studied cytokines. SARS-CoV-2 host cell protease TMPRSS2 also presented correlations with CD8+ T-cells and NK cells in lung tissue. It is suggested that lung cell SARS-CoV-2 infection stimulates cytotoxic lymphocytes and its attractant cytokines, which presents significance for prevention of severe COVID-19 symptoms. Furthermore, high and pre-existing ACE2 and TMPRSS2 expression may be associated with severe COVID-19 responses. This research contributes to understanding the variation of COVID-19 infection and severity of symptoms from a molecular immunology perspective.
Journal Article: Duijf 2020. Low Baseline Pulmonary Levels of Cytotoxic Lymphocytes as a Predisposing Risk Factor for Severe COVID-19. Host-Microbe Biology ASM
Summary by Rebecca Ng










