Autoimmune encephalitis (AE) is a severe and complex condition characterized by inflammation of the brain, leading to symptoms such as seizures, cognitive decline, and movement disorders. A recent study, published in the Journal of Neuro-immunology in 2024, explores a novel subtype of AE: unilateral cortical autoimmune encephalitis. This form of AE features strictly unilateral inflammation, which is an unusual anatomical presentation. The study reviews 12 cases, comparing this subtype to late-onset Rasmussen’s encephalitis (LoRE).
Additional reading: New Study Links Inflammation and Blood-Brain Barrier Dysfunction to Down Syndrome Regression Disorder
Study Design and Patient Characteristics
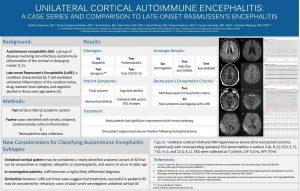
The research involved a retrospective review of patients from two academic centers: Case Western Reserve University and New York University Langone Health. Patients included in the study exhibited unilateral cortical inflammation confirmed through MRI and/or EEG. The average age of patients was 65 years, and 58% were female. Importantly, most patients were seronegative for neuronal antibodies, a finding that is more common in idiopathic cases of autoimmune encephalitis.
While six patients had idiopathic cases of AE, others had more identifiable causes: two were post-COVID-19 cases, and two were paraneoplastic or iatrogenic (linked to immune checkpoint inhibitors). The most common symptoms included focal seizures (seen in nine patients), cognitive decline, hemicortical deficits, and movement disorders, such as dystonia and hemichorea.
Comparisons to Rasmussen’s Encephalitis (RE)
Rasmussen’s encephalitis is typically a childhood condition that involves unilateral brain inflammation and drug-resistant seizures. Late-onset RE (LoRE) shares similar features but occurs in adults. In this study, five patients met the criteria for LoRE, but others had overlapping features without fully meeting the diagnostic criteria. Like LoRE, these patients showed progressive cortical atrophy and seizures that were difficult to control.
What makes unilateral cortical AE particularly noteworthy is its responsiveness to immunotherapy. Patients received treatments including corticosteroids, intravenous immunoglobulin (IVIG), rituximab, and cyclophosphamide. Most patients showed significant improvement, with five achieving complete seizure control and cognitive recovery. In refractory cases, surgical interventions such as functional hemispherectomy were considered, leading to seizure freedom but with some residual cognitive or motor deficits.
Clinical Implications
This study highlights a novel subtype of autoimmune encephalitis that predominantly affects older adults and presents with unique anatomical and clinical features. While it shares similarities with LoRE, unilateral cortical AE appears more amenable to immunotherapy, which may offer new hope for patients suffering from this condition.
The findings also suggest that clinicians should consider unilateral cortical AE in the differential diagnosis of older patients presenting with focal seizures and cognitive decline, especially when MRI findings show unilateral inflammation. Further research is needed to fully understand the long-term outcomes and the potential role of advanced therapies in refractory cases.
Conclusion
Unilateral cortical autoimmune encephalitis is a rare but treatable condition, distinct from other forms of AE. Its responsiveness to immunotherapy distinguishes it from more refractory forms like Rasmussen’s encephalitis. Early diagnosis and targeted therapy are key to improving patient outcomes, and this study offers valuable insights for clinicians managing similar cases in the future.
Summary by Faith Oluwamakinde