Idiopathic Interstitial Pneumonia (IIP) is a complex group of lung diseases without a known cause, often resulting in progressive lung fibrosis. Unlike interstitial lung disease (ILD) associated with connective tissue diseases, IIP lacks a clear systemic cause and often requires extensive investigation. Recent research has identified a novel biomarker, the anti-IFI16 antibody, which appears to be specifically associated with certain cases of IIP and may hold clinical significance as a prognostic indicator.
The study involved screening serum samples from 295 patients with IIP to detect autoantibodies using a protein array and immunoprecipitation assays. Researchers identified anti-IFI16 antibodies in a small subset of patients, confirming that interferon gamma-inducible protein 16 (IFI16) is a novel autoantigen in IIP. This antibody has previously been linked to autoimmune diseases, such as systemic lupus erythematosus and systemic sclerosis, but had not been explored in IIP cases until now. The presence of anti-IFI16 was associated with poorer outcomes, as these patients were less likely to receive immunosuppressive therapy and had significantly lower survival rates compared to those with other autoantibodies, such as anti-aminoacyl tRNA synthetase (ARS) antibodies.

Fig. 1. Enrollment and selection of patients.
This study enrolled 295 patients diagnosed with idiopathic interstitial pneumonia of the 308 patients from five institutions. Thirteen patients were excluded because they were diagnosed with connective tissue disease during the observation period. The most common diagnosis was unclassifiable IIP (58 %), followed by IPF (31 %), NSIP (5 %), PPFE (3 %), COP (2 %), DIP (1 %), and RB-ILD (0 %). Abbreviations: RA, rheumatoid arthritis; SjS, Sjogren syndrome; DM, dermatomyositis; PMR, polymyalgia rheumatica; RP, relapsing polychondritis; IFI16, interferon gamma-inducible protein 16; ARS, aminoacyl-tRNA synthetase; IPAF, interstitial pneumonia with autoimmune features; IPF, idiopathic pulmonary fibrosis; NSIP, non-specific interstitial pneumonia; PPFE, pleuroparenchymal fibroelastosis; COP, cryptogenic organizing pneumonia; DIP, desquamative interstitial pneumonia; RB-ILD, respiratory bronchiolitis-associated interstitial lung disease.
Patients with anti-IFI16 antibodies exhibited unique immunologic features, including an interferon pathway activation linked to pro-inflammatory cytokine production and type 1 interferon release. This immune response may underlie the lung tissue damage and fibrosis seen in these patients, suggesting that anti-IFI16 is not only a marker but potentially a driver of disease pathology in IIP. The researchers also noted that IFI16 expression was elevated in airway epithelial and immune cells, indicating that IFI16-related immune activation may play a role in the inflammation and tissue remodeling associated with IIP.
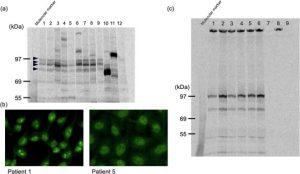
Fig. 2. Immunoprecipitation and indirect immunofluorescence with patient sera.
(a) Using 35S-methionine-labeled HeLa cell extracts, tetrameric bands at a molecular weight of approximately 100 kDa were immunoprecipitated. Lane 1–9, patient sera; Lane 10, anti-PL-7 antibody (approximately 80 kDa)–positive serum; Lane 11, anti-PL-12 antibody (approximately 110 kDa)-positive serum; Lane 12, healthy control. Arrowheads show the tetrameric bands.
(b) An indirect immunofluorescent staining pattern on HEp-2 cell slides produced by a serum positive for anti-tetramer antibody (Patients 1 and 5 in Table 2). Patient 1 showed a nucleolar pattern, and Patient 5 showed a speckled pattern.
(c) Immunoprecipitation analysis of in vitro translated interferon-gamma inducible protein 16 (IFI16). IFI16 protein from a plasmid encoding IFI16 cDNA was expressed in vitro and immunoprecipitated using patients and healthy control. Lanes 1 to 6 correspond to patients 1 to 6 in Table 2, respectively. Sera from healthy control patients (negative control) are shown in lanes 7 to 9.
From a clinical perspective, the identification of anti-IFI16 antibodies in IIP patients offers new insights into stratifying patients based on their likely disease progression. By incorporating anti-IFI16 testing into routine diagnostics, physicians could better identify patients who may benefit from early intervention with immunosuppressive or anti-fibrotic therapies. This biomarker represents an important step in refining treatment strategies for IIP, particularly for those with a high risk of acute exacerbations or progressive lung function decline.
Summary by Faith Oluwamakinde










