“Applying their immune monitoring experience (see image below) to large patient cohorts hospitalised at Mount Sinai in New York during the COVID-19 epidemic, Sacha Gnjatic and his team investigated cytokine and antibody profiles.” (Source: IUIS Webinars Page)
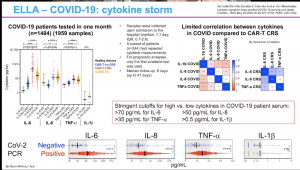 Based on the heterogeneity of COVID-19 pathology, Sacha and colleagues hypothesised that cytokines such as IL-6, IL-8, IL-1β and TNF could potentially predict disease severity and outcome. Sacha demonstrated that IL-6, IL-8 and TNF, individually and when combined in a model, correlate with various aspects of disease severity and survival outcome. Even though disease severity was also associated with high IL-β levels, the predictive value of this cytokine was low. Based on these results targeting these cytokines using immunotherapy could potentially improve morbidity and fatality, however, clinicians should be mindful of when to give such therapy as it could cause more harm. (Read More: Del Valle et al., 2020 Pre-print)
Based on the heterogeneity of COVID-19 pathology, Sacha and colleagues hypothesised that cytokines such as IL-6, IL-8, IL-1β and TNF could potentially predict disease severity and outcome. Sacha demonstrated that IL-6, IL-8 and TNF, individually and when combined in a model, correlate with various aspects of disease severity and survival outcome. Even though disease severity was also associated with high IL-β levels, the predictive value of this cytokine was low. Based on these results targeting these cytokines using immunotherapy could potentially improve morbidity and fatality, however, clinicians should be mindful of when to give such therapy as it could cause more harm. (Read More: Del Valle et al., 2020 Pre-print)
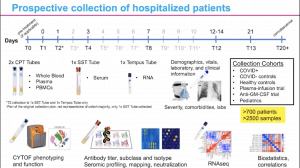 He also briefly described an ongoing (prospective, longitudinal) study (n>700) that aims to utilise cellular (mass cytometry), serum (Olink), antibody (mapping, neutralisation) and transcriptomic (RNA-Seq) profiling to identify potential cellular clusters associated with severity. As observed with single measurements, IL-6, IL-8 and TNF were associated with disease severity. Lastly, Sacha presented data on IgM, IgG, IgA, IgG1, IgG2, IgG3 antibody profiling (n>260, using high-throughput ELISA of the large cohort). He showed that the antibody subclasses and subtypes specific for the same antigen correlate with each other. He also reported a positive correlation between disease severity and high IgG, IgA, IgG1 and IgG3 titres. These high titres could be a consequence of duration of disease and higher viral load, and not necessarily indicative of antibody-dependent enhancement of disease.
He also briefly described an ongoing (prospective, longitudinal) study (n>700) that aims to utilise cellular (mass cytometry), serum (Olink), antibody (mapping, neutralisation) and transcriptomic (RNA-Seq) profiling to identify potential cellular clusters associated with severity. As observed with single measurements, IL-6, IL-8 and TNF were associated with disease severity. Lastly, Sacha presented data on IgM, IgG, IgA, IgG1, IgG2, IgG3 antibody profiling (n>260, using high-throughput ELISA of the large cohort). He showed that the antibody subclasses and subtypes specific for the same antigen correlate with each other. He also reported a positive correlation between disease severity and high IgG, IgA, IgG1 and IgG3 titres. These high titres could be a consequence of duration of disease and higher viral load, and not necessarily indicative of antibody-dependent enhancement of disease.
Summary by Cheleka Mpande










