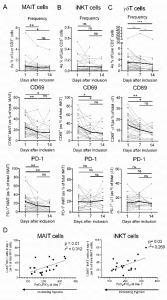
Kinetic analysis of the frequency and phenotype of innate T cells in severe Covid-19 patients. A-C, Flow cytometry analyses of relative proportion and CD69 and PD-1 expression on MAIT (A), γδT (B) and iNKT (C) cells in the blood of critically ill Covid-19 patients at days 1 (n = 30), 7 (n = 27) and 14 (n = 14). Kinetics plots showing mean value for each patient(each greyline corresponds to one patient). Median values for each parameters439were plotted in black. D, Spearman’s rank correlation of CD69 expression on blood iT cells and hypoxia levels in Covid-19 patients. ns, not significant; *, p<0.05; **, p<0.01; ***, p<0.001.
COVID-19 and SARS-CoV-2 immunological research has predominantly focused on the role of innate cells such as macrophages, NK, neutrophils, and adaptive cellular and humoral immunity in pathogenesis. Recent Pre-print by Jouan and colleagues analysed the biology of innate T cells: mucosal associated invariant T (MAIT) cells, γδ T and invariant natural killer (iNK) T cells in critically ill COVID-19 patients with varying co-morbidities (46.7% with Hypertension; 30% with Type 2 diabetes; 10% with cardiovascular disease).
Researchers observed that innate T cells from COVID-19 patients were highly pro-inflammatory characterised by high expression of IL-17 but not IFN-g, compared to healthy controls. Interestingly, MAIT cells and iNKT cells from COVID-19 patients expressed high levels of both CD69 and PD-1, markers associated with activation and exhaustion, respectively. Based on this, and other evidence described in the Pre-print author concluded that sever COVID-19 is associated with “an altered innate T cell biology that may account for the dysregulated immune response observed in COVID-19-related acute respiratory distress syndrome.”
Journal Article: Jouan et al. Pre-print. Functional alteration of innate T cells in critically ill Covid-19 patients. MedRxiv
Summary by Cheleka Mpande










