Produced naturally in the skin through sunlight exposure, vitamin D influences many biological pathways. In the immune system, it particularly affects the communication between dendritic cells, specialised immune cells that help initiate responses, and T cells, which are the immune system’s primary defence.
Normally, T cells help fight infections. However, in autoimmune diseases, they mistakenly target the body’s healthy tissues, leading to chronic inflammation and damage.
Vitamin D is often celebrated for its role in bone health and general well-being, but new research reveals it also plays a critical role in regulating the immune system (Figure 1). The findings shed light on why low vitamin D levels have long been linked to autoimmune diseases, including multiple sclerosis (MS).
The study highlights a molecular mechanism through which vitamin D tempers the immune response, potentially reducing the risk of the body attacking its own tissues.
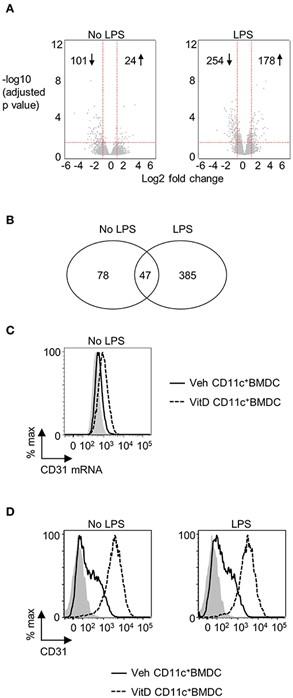
Figure 1. CD31 is upregulated by 1,25(OH)2D3 in BMDC. Bone marrow derived dendritic cells (BMDC) were generated over 9 days in the presence of 1,25(OH)2D3 (VitD) or absence (Veh) of 20 mM 1,25(OH)2D3. (A) Veh and VitD BMDC were matured for 18 h in the presence or absence of 0.1 μg/ml LPS. mRNA was extracted and microarray performed. Differential gene expression caused by 1,25(OH)2D3 in the absence (left) or presence of LPS stimulation (right) is depicted as volcano plots. (B) Number of genes differentially regulated by 1,25(OH)2D3 in CD11c+BMDC in the presence or absence of LPS stimulation. (C) Representative flow plot of CD31 mRNA levels in Veh (continuous line) and VitD (dashed line) CD11c+BMDC as assessed by PrimeFlow. Fluorescence minus one is indicated by gray shaded area. n = 3. (D) Representative flow plots of CD31 protein expression in Veh (continuous line) and VitD (dashed line) CD11c+BMDC in the absence (left panel) or presence (right panel) of LPS stimulation as assessed by flow cytometry. Isotype control is indicated by gray shaded area.
The team studied cells from both mice and humans to understand how vitamin D alters immune signalling. They discovered that vitamin D prompts dendritic cells to produce more of a surface molecule called CD31. CD31 acts as a kind of molecular “brake” by preventing stable contact between dendritic cells and T cells, a critical step required for T cell activation. Without this sustained interaction, T cells are far less likely to trigger a strong immune response. The results – A dampened immune reaction, which in healthy conditions may help prevent overactivation that could lead to autoimmune attacks.
This mechanism helps explain why vitamin D deficiency has been repeatedly associated with a higher risk of autoimmune conditions, including MS. When vitamin D levels are low, dendritic cells may fail to express enough CD31, allowing for greater T cell activation and, potentially, harmful immune responses against the body’s own tissues.
These findings not only provide a biological explanation for epidemiological links between vitamin D and autoimmune disease but also point toward potential therapeutic strategies.
As scientists continue to investigate the interplay between environmental factors, immunity, and disease susceptibility, this study highlights how something as simple as sunlight exposure and vitamin D levels can have profound impacts on immune health.
Journal article: Saul, L., et al. 2025. 1,25-Dihydroxyvitamin D3 Restrains CD4+ T Cell Priming Ability of CD11c+ Dendritic Cells by Upregulating Expression of CD31. Frontiers in Immunology.
Summary by Stefan Botha