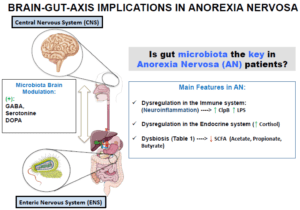
Microbiota as a recruiter of bidirectional communication between the brain and gut, and changes in microbiota composition observed in Anorexia Nervosa patients. (Source: Mendez-Figueroa et al., Microogranisms 2019)
Evidence emerging from the field of psychoneuroimmunology has supported a so-called “Immunology hypothesis” in psychiatry, whereby immunological dysfunction forms the biological aetiology of a subset of mental illnesses such as depression, anxiety, schizophrenia, and more recently, eating disorders. Large population-based and laboratory studies have illuminated the positive association between immune-dysfunction and the onset risk of eating disorders, such as anorexia nervosa (Favaro et al., Setiawan et al.,)
The brain and the immune system can communicate with each other in a few different ways. One way is through neural projections of the vagal and trigeminal nerves into different structures of the brain responsible for behaviour and emotion. These nerves can be activated through peripherally-produced pathogen-associated molecular patterns (PAMPs) and inflammatory cytokines. Additionally, PAMPS and inflammatory cytokines also circulate and enter regions of the brain through volume diffusion, may potentially underlie well-documented associations between chronic inflammatory disorders (type 2 diabetes, rheumatoid arthritis, cardiovascular disease) and major depressive disorders.
As a result, infections and inflammatory processes has gained strong momentum in understanding mental illnesses, including eating disorders. In this study published in the Journal of the American Medical Association (JAMA) Psychiatry, Breithaupt et al. investigated the association between childhood infections with subsequently diagnosed eating disorders (anorexia nervosa, bulimia nervosa, eating disorder not otherwise specified) in a large population-based cohort of females. They demonstrated a significantly elevated risk of an eating disorder diagnosis following hospitalization for infections, which followed a dose-response association between number of hospitalization for infections and onset of diagnosis.
Breithaupt et al. suggested a few mechanisms underlying this association, including increased levels of pro-inflammatory cytokines (TNF-a, IL-1, IL-6), which is also produced by gastrointestinal inflammatory disorders such as Crohn’s disease, that may contribute to projections to brain structures involved in appetite suppression and weight loss.
In summary, these profound clinical epidemiology findings [3] linking eating disorders to potential immune mechanisms supports the emerging immunology hypothesis behind mood/eating disorders and thus, holds great potential for future treatment, prevention, and stigma-reduction efforts in current mental disorder research and advocacy.
Journal Article: Breithaupt L, Köhler-Forsberg O, Larsen JT, et al. 2019 Association of Exposure to Infections in Childhood With Risk of Eating Disorders in Adolescent Girls. JAMA Psychiatry.
Article by Bryan Gascon











