New research links oral bacteria to disability severity in MS, pointing to a possible “oral–brain axis” (Table 1).
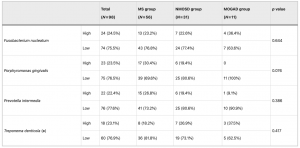
Table 1: Proportion of patients with high and low relative abundances of periodontal pathogens stratified by central inflammatory demyelinating disease. MS, multiple sclerosis; NMOSD, neuromyelitis optica spectrum disorder; MOGAD, myelin oligodendrocyte glycoprotein antibody-associated disease. High and low abundances were defined using the third quartile (Q3) cutoff for the ΔΔCt-calculated relative abundance. High = top 25%, low = below Q3. (※) For Treponema denticola, the total number of evaluated patients was lower than the total number of patients in each disease group because several samples did not yield valid Ct values by qPCR and were thus considered nondetectable. As a result, the total number of patients evaluated for this pathogen was 78 (MS patients 44; NMOSD patients 26; MOGAD patients 8).
Chronic inflammation is increasingly recognized as a contributor to diseases of the central nervous system. Now, a new study suggests that periodontal disease, and the bacteria that drive it, may be linked to the severity of multiple sclerosis (MS).
Researchers found that MS patients with higher levels of a common oral bacterium, Fusobacterium nucleatum, were significantly more likely to have moderate to severe neurological disability. The association was not observed in related autoimmune conditions, highlighting a potential MS-specific link between oral inflammation and disease progression.
The gut microbiome has been extensively studied in MS, but the oral microbiome has received far less attention. Yet the mouth is a major source of chronic inflammation, particularly in periodontal disease, which affects up to 60% of adults worldwide.
Periodontitis has already been linked to conditions such as cardiovascular disease, diabetes, and rheumatoid arthritis. The new findings raise the possibility that oral bacteria may also influence neuroinflammatory diseases.
The researchers analysed tongue-coating samples from patients with:
- Multiple sclerosis (MS)
- Neuromyelitis optica spectrum disorder (NMOSD)
- Myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD)
They quantified periodontal bacteria and classified patients as having high or low relative abundance based on population distribution. Clinical disability was measured using the Expanded Disability Status Scale (EDSS).
The results were:
- MS patients with high levels of Fusobacterium nucleatum were far more likely to have EDSS ≥ 4, indicating moderate to severe disability
- After adjusting for age, disease duration, relapse history, and MS subtype, these patients had ~10-fold higher odds of severe disability
- Nearly 62% of MS patients with high F. nucleatum levels had moderate-to-severe disability, compared with ~19% of those with lower levels
Importantly, no similar association was seen in NMOSD or MOGAD, suggesting a disease-specific effect in MS.
Fusobacterium nucleatum is known as a “bridge bacterium” in dental biofilms, helping different bacterial communities adhere and persist. The researchers propose that it may play a similar role biologically, linking oral inflammation to systemic immune activation and neuroinflammation.
Patients who harboured F. nucleatum together with other periodontal pathogens showed even greater disability, reinforcing the idea that bacterial communities, not single microbes alone, may influence disease severity.
These findings ask the question:
- Could improved oral hygiene or periodontal treatment slow disability progression?
- Might oral bacteria serve as biomarkers for disease severity or progression risk?
A common periodontal bacterium, Fusobacterium nucleatum, is associated with greater disability in multiple sclerosis, but not in related neurological disorders. The findings suggest that chronic oral inflammation may influence MS progression, raising the possibility that dental health could become part of future MS management strategies.
Journal article: Naito, H. et al. 2025. The periodontal pathogen Fusobacterium nucleatum is associated with disease severity in multiple sclerosis, Scientific Reports.
Summary by Stefan Botha










