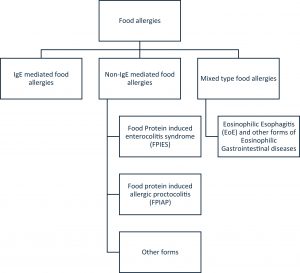
New ANAcare report offers clinicians a practical roadmap for accurate, consistent diagnosis of IgE-mediated food allergy (Figure 1).
Diagnosing food allergies remains one of the most challenging areas in clinical allergy practice. Despite clear evidence-based guidelines, real-world diagnosis varies widely between countries and even between clinics in the same region. A new report from the Global Network of Centres of Excellence for Anaphylaxis & Food Allergy (ANAcare) aims to change this by offering a unified, operational pathway to help clinicians translate guidance into consistent, accurate diagnostic care.
Why Food Allergy Diagnosis Is So Variable
International guidelines outline best practices, but implementation differs markedly due to:
- Differences in test availability and laboratory access
- Variation in clinical thresholds for performing oral food challenges
- Staffing limitations and resource constraints
- Local traditions or preferences in diagnostic practice
As a result, both underdiagnosis and overdiagnosis remain common. Skin prick tests and serum-specific IgE levels, while essential tools, are often misinterpreted without a careful clinical history, leading to unnecessary food avoidance or missed diagnoses.
To address this gap, ANAcare reviewed global allergy guidelines, incorporated emerging evidence, and gathered input from clinicians across 13 countries. The resulting pathway provides:
- Structured guidance for taking a detailed allergy history
- Standardized advice on when and how to use sensitisation tests
- Clear criteria for deciding when oral food challenges are essential
- Emphasis that sensitisation ≠ clinical allergy, reinforcing the need to link test results with symptoms
The approach focuses on how to apply guidelines, not simply what they say, making it accessible for clinicians in diverse settings.
Overcoming Real-World Barriers
The report directly addresses the practical challenges that often limit guideline adoption:
- Shortage of trained allergy specialists
- Limited capacity to safely perform oral food challenges
- Variability in testing quality and interpretation
- Differences in reimbursement or national health policy
By presenting a step-by-step operational tool, ANAcare aims to harmonize diagnostic practice for centres with varying levels of experience and resources.
Accurate diagnosis is vital to avoid unnecessary dietary restrictions, support healthy nutrition, and ensure patients receive appropriate emergency plans and education. The pathway is designed not only for specialty centres but also for primary care, paediatricians, emergency clinicians, and general hospital teams, the first point of contact for many families.
The authors also highlight that widespread adoption of a standardized pathway will improve comparability of data between centres worldwide, strengthening future allergy research and improving patient care on a global scale.
Developed by allergists, immunologists, dieticians, psychologists, and guideline experts, the ANAcare pathway represents a strong international consensus on how to operationalise evidence-based allergy diagnosis. Even if clinics cannot offer every diagnostic step, the shared framework helps guide appropriate referral, reduce diagnostic confusion, and build capacity over time.
Journal article: Venter C, et al. 2025. Diagnosing IgE-mediated food allergy: How to apply the latest guidelines in clinical practice. J Allergy Clin Immunol Glob.
Summary by Stefan Botha