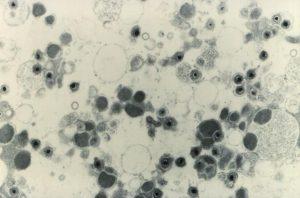
Cytomegalovirus (CMV) is a chronic viral infection and part of the herpesvirus group, and is associated with a decreased CD4/CD8 ratio and increased systemic inflammation. Most notably, CMV infection is also associated with increased expansion of terminally differentiated T cells. HIV-CMV co-infection is quite high among HIV-infected individuals, where CMV infection may drive the ‘immune senescent’ phenotype.
Researchers from the Netherlands and UK participated as part of the Co-morBidity in Relation to AIDS (COBRA) collaboration to evaluate activation and terminal differentiation of T cells in HIV patients on ART. The COBRA cohort was used to assess treated HIV infection. Peripheral blood mononuclear cell (PBMC) samples were used to determine the expression of T cell differentiation through naïve, central memory, effector memory, transitional memory, and terminally differentiated effector memory. In contrast, T cell activation was evaluated through the proportion of CD38 and HLA-DR within CD4 or CD8 T cell populations. Additionally, CMV reactivation, recurrent CMV antigen exposure, and antibody maturation was determined.
Results indicated that HIV-positive participants were more likely to be infected with CMV than their HIV-negative counterparts. Despite being on ART, HIV-positive participants had incomplete CD4+ T-cell restoration and increased CD8 T cell counts. T cell activation was higher in HIV-positive (with ART) participants. Furthermore, HIV-positive individuals had lowered naïve CD4+ and effector memory CD8+ cells, but no differences associated with the other types of cells analyzed. However, when comparing HIV-positive participants to blood bank donor cells, there was a higher percentage of effector memory CD4+ and CD8+ cells. Through linear regression analysis, it was determined that both CMV infection and HIV infection were independently associated with T cell activation, exhaustion, and terminal differentiation. HIV infection was associated with increased T cell exhaustion, while CMV infection was associated with decreased CD8+ T cell exhaustion. Lastly, HIV-positive participants had increased total and high avidity CMV antibody titers.
The authors of this study demonstrated that HIV-positive participants individuals face several differences in immune-associated cells. However, CMV infection may explain higher levels of terminally differentiated T cells in both HIV-positive and HIV-negative populations. The multiple regression analysis uncovered the underlying variable of CMV infection, which may be responsible for influencing T cell terminal differentiation during HIV infection. This wide-ranging study provides insight of the impact of infectious disease on T cell developmental biology.
Article by Rebecca Ng