Researchers uncover “pseudo leukotrienes” that could reshape how asthma and inflammatory diseases are treated (Figure 1).
For decades, asthma has been explained by a familiar culprit: leukotrienes, inflammatory molecules released by immune cells that constrict airways and make breathing difficult. Entire classes of asthma drugs have been designed to block their effects, and for many patients, these treatments help.
But new research suggests the story may be more complex. In a new study scientists report the discovery of previously unrecognized molecules that closely resemble leukotrienes but are produced through a completely different chemical pathway. These newly identified compounds, dubbed “pseudo leukotrienes,” may be the true drivers of inflammation in asthma.
Classic leukotrienes are generated through tightly regulated enzymatic reactions. In contrast, pseudo leukotrienes arise from free radical–driven lipid oxidation, a chaotic chemical process like combustion.
People with asthma may lack sufficient antioxidant defences to neutralize free radicals, allowing these reactions to spiral and generate large quantities of pseudo leukotrienes. Despite their different origins, both leukotrienes and pseudo leukotrienes activate the same airway receptors, triggering inflammation and bronchoconstriction.
Current asthma drugs, such as leukotriene receptor blockers, work by blocking the receptor, preventing inflammatory molecules from “turning the ignition.” But if pseudo leukotrienes are the dominant inflammatory signal, blocking the receptor may also interfere with beneficial roles of leukotrienes, which contribute to normal immune responses, healing, and even brain function.
This shift opens the door to antioxidant or redox-targeted therapies that selectively dampen harmful inflammation without suppressing beneficial immune functions.
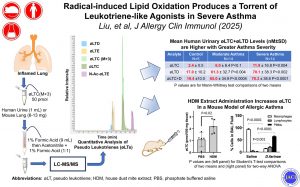
To test their hypothesis, the researchers synthesized pseudo leukotrienes in the lab and developed methods to detect them in biological samples. They then analysed urine from people with mild and severe asthma and compared it to samples from healthy controls.
The results:
- Pseudo leukotrienes were present at much higher levels in asthma patients
- Levels correlated strongly with disease severity
- Even mild asthma patients had four to five times higher levels than healthy individuals
This suggests pseudo leukotrienes could serve as a new biomarker for asthma severity and treatment response.
The team now plans to investigate whether pseudo leukotrienes contribute to other inflammatory diseases, including RSV infection, bronchiolitis in infants, chronic obstructive pulmonary disease (COPD) and potentially even neurodegenerative conditions such as Parkinson’s and Alzheimer’s disease.
Researchers have identified a new class of inflammatory molecules, pseudo leukotrienes that may be the real drivers of asthma. By targeting the oxidative processes that generate them, future therapies could treat asthma more precisely while preserving the body’s beneficial inflammatory responses.
Journal article: Liu, S.-Y., et al. 2025. Radical-induced Lipid Oxidation Produces a Torrent of Leukotriene-like Agonists in Severe Asthma. Journal of Allergy and Clinical Immunology.
Summary by Stefan Botha