In this summary, we focus on the IUIS-Immunopaedia-Frontiers webinar talk by Eric Vivier on Harnessing innate immunity from cancer therapy to COVID-19.
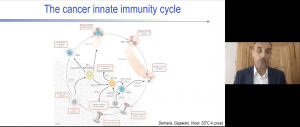 Eric Vivier began his talk by giving an overview of why targeting innate cells may improve cancer immunotherapy. He showed that Natural killer (NK) cells play a role in immune responses against cancer. Besides directly killing cancer cells independently or via antibody-dependent cellular cytotoxicity (ADCC), NK cells also release cytokines and chemokines which activate other innate cells involved in the induction of T cell-mediated immunity.
Eric Vivier began his talk by giving an overview of why targeting innate cells may improve cancer immunotherapy. He showed that Natural killer (NK) cells play a role in immune responses against cancer. Besides directly killing cancer cells independently or via antibody-dependent cellular cytotoxicity (ADCC), NK cells also release cytokines and chemokines which activate other innate cells involved in the induction of T cell-mediated immunity.
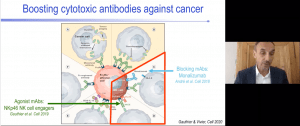 He gave an overview of the immunological basis of monoclonal antibodies, Monalizumab and Cetuximab, that target different aspects of NK mediated immune responses. Monalizumab prevents the inhibition of NK/CD8 T cell activity my tumour cells by preventing the binding of HLA-E on tumour cells to NKG2A on NK/CD8 T cells, while Cetuximab improves NK cell anti-tumour immune responses by recognising EGFR (molecule overexpressed on tumours cells) and binding to the FcgRIII/CD16 on NK cells activating NK cell-mediated ADCC. He then described a novel immunotherapy based on NKp46 NK cell engagers (NKCEs). This molecule can recognise tumour antigens and bind to both FcgRIII/CD16 and NKp46 receptor on NK cells resulting in ADCC and the release of cytokines/chemokines that contribute to the induction of adaptive T cells. He provided preliminary evidence that suggests that NKCEs could have a superior activity to current immunotherapies available.
He gave an overview of the immunological basis of monoclonal antibodies, Monalizumab and Cetuximab, that target different aspects of NK mediated immune responses. Monalizumab prevents the inhibition of NK/CD8 T cell activity my tumour cells by preventing the binding of HLA-E on tumour cells to NKG2A on NK/CD8 T cells, while Cetuximab improves NK cell anti-tumour immune responses by recognising EGFR (molecule overexpressed on tumours cells) and binding to the FcgRIII/CD16 on NK cells activating NK cell-mediated ADCC. He then described a novel immunotherapy based on NKp46 NK cell engagers (NKCEs). This molecule can recognise tumour antigens and bind to both FcgRIII/CD16 and NKp46 receptor on NK cells resulting in ADCC and the release of cytokines/chemokines that contribute to the induction of adaptive T cells. He provided preliminary evidence that suggests that NKCEs could have a superior activity to current immunotherapies available.
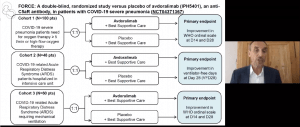
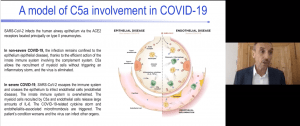 Last year Eric Vivier gave an IUIS webinar talk on Involvement of C5a-C5aR1 axis in COVID-19 pathology (read summary for more details). C5a plays a role in driving the pathogenesis of influenza-induced pneumonia and Acute respiratory distress syndrome (ARDS) by promoting infiltration of neutrophils and macrophages that get activated by a hyperinflammatory cytokine micro-environment. He then presented work that demonstrated that blocking of C5a activity using avdovalimab (anti-C5aR1 monoclonal antibody) reduces neutrophil migration and acute lung injury using a murine model. They are currently testing the utility of this immunotherapy against severe COVID-19 in clinical trials.
Last year Eric Vivier gave an IUIS webinar talk on Involvement of C5a-C5aR1 axis in COVID-19 pathology (read summary for more details). C5a plays a role in driving the pathogenesis of influenza-induced pneumonia and Acute respiratory distress syndrome (ARDS) by promoting infiltration of neutrophils and macrophages that get activated by a hyperinflammatory cytokine micro-environment. He then presented work that demonstrated that blocking of C5a activity using avdovalimab (anti-C5aR1 monoclonal antibody) reduces neutrophil migration and acute lung injury using a murine model. They are currently testing the utility of this immunotherapy against severe COVID-19 in clinical trials.
Summary by Cheleka AM Mpande